Considerations in the Development of the Lower Limb in Children
Learning to conduct a thorough biomechanical evaluation of a child can be a rewarding activity. It is an important skill in our profession as the earlier the detection of an abnormality, the better chances of managing or correcting it without surgery, and many biomechanical issues patients present with later in life are traceable to anomalies in their development. In fact, the origin of the word orthopaedic from Greek is orthos—right or straight, and paideia—the rearing of children. When growth plates are still open, and structures are not yet fully formed, orthotic interventions along with physical therapy can be used to influence development and gait. In much the same way that retainers and dental braces are used to straighten children’s teeth, orthotists and pedorthists can provide results that last a lifetime. To become skillful, good clinicians must have an understanding of normal and abnormal development of the lower limb (Table 1).
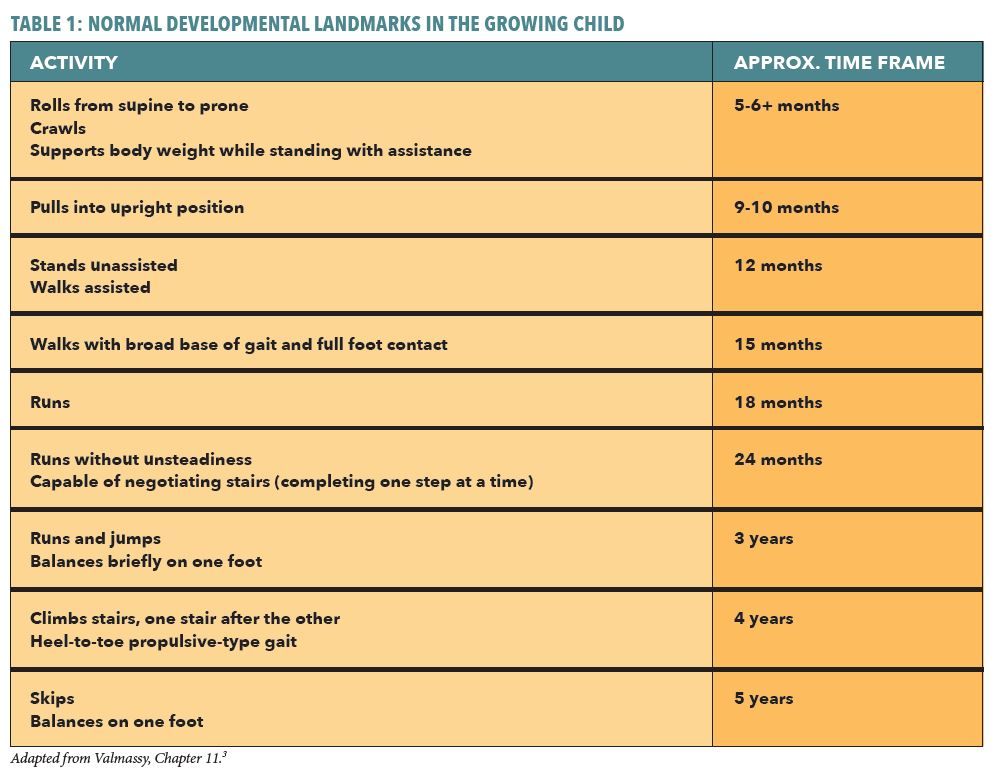
Significant deviation from these established developmental landmarks may indicate more serious neuromuscular, musculoskeletal, or syndrome disorders that should be immediately referred for further investigation.
Often children are brought to the clinic for evaluation in response to a parent’s concern that “something doesn’t look right.” This may be the appearance of an awkward-looking gait,
asymmetry, or reports of tripping, falling, or the child being uncoordinated or clumsy. In the evaluation, it is good to determine if the child complains of tiredness, fatigue, or pain after running around. He or she may be less active than his or her peers, preferring to sit out sports or other play. Even if the cause is benign, it is essential to treat the issue seriously as all children should be encouraged to participate in games, sports, and other activities to develop the essential lifelong habit of physical fitness. It is also helpful to consider familial history, including parents and siblings. Although a deformity may not be hereditary, an underlying contributing factor such as ligamentous laxity may be. Each child should be given a complete regular biomechanical exam that checks muscle strength and range of motion (ROM) at the major joints. However, it is also important to have knowledge of the significant changes and rapid development that children undergo, especially in the early years up to age seven.
Hip Motion
Hip ROM should be checked in the transverse plane with the child seated. This test can be done with the knee extended and a dot sticker placed on the knee. Rotate the leg clockwise and counterclockwise. Noting the motion at the knee, record the degree of rotation. Up to ages six and seven, there will be significant motion available, and greater external than internal rotation. Gradually the range of internal and external rotations should even out to approximately 80 degrees total ROM (i.e., 40 degrees internal and 40 degrees external). Repeat the test with the knee flexed and be sensitive to the feel of the end ROM. If there is a significant difference between the measurements accompanied with a soft or spongy feel to the end ROM, this indicates a muscle or ligament may be contributing to a restriction. If the end ROM is abrupt, it is more likely due to a bony block. There are several other important tests to evaluate hip motion in different planes, and the examiner must remain alert for any sign of a dislocation.
Femoral inclination is the angle, in the frontal plane, between the long axis of the head and neck and the long axis of the shaft. Infants have a high angle of inclination (140 – 150 degrees) that decreases with time. By age six the inclination angle averages 128 degrees. Coxa vara exists when the angle is less than this and coxa valga occurs when the angle remains higher. Photograph courtesy of Gray’s Anatomy 1918 edition.
Patellae and Foot Position
Until children reach ages between five and six, they usually demonstrate external limb rotation, and the practitioner should first verify there is no asymmetry. Over time there is a gradual rotation of the patellae towards the frontal plane. Likewise, a mild in-toeing foot position should be noted as being within normal range, symmetrical, and decreasing as the child develops. Asymmetry of either patellar or foot position is a clue to an underlying issue.
In the early years, the femur and tibia have inherent rotations due to a combination of torsion and position. Torsion of a long bone refers to increased rotation about the longitudinal axis and is an osseous abnormality. Position of a bone describes the attitude of the bone as a result of soft tissue or muscular forces. Often torsion and position are present together, each playing a role influencing limb rotation. Torsion is structural whereas position is functional and may only show up dynamically when the child walks or runs.
Anteversion means “rotated forward” and refers to the orientation of the femoral neck and head in relation to the condyles at the knee. Typically, at birth there is a noticeable internal angulation, and this gradually reduces to 8-12 degrees in adults. Internally facing patellae indicate femoral anteversion due to internal torsion. However, if both patellae face forward on the frontal plane but the feet are adducted, then there is likely either internal tibial torsion or position, or a metatarsus adductus. It is also not uncommon to see combinations of these factors present together. Metatarsus adductus is a common pediatric abnormality, which responds well to early conservative treatment. However, if missed or ignored, it can lead to problems later in life such as a prominent and painful base of the fifth metatarsal, difficulty with shoe fitting, and perhaps early hallux valgus.
Knee Position
Normal infants and children up to the age of four appear bowlegged. The genu varum is a result of lateral bowing of the long bones, plus the exaggerated angle of the femoral head and neck in relation to the shaft (coxa valga). This femoral angle of inclination decreases by approximately 20 degrees by age six. If marked genu varum persists beyond age four, further examination is required to rule out diseases such as Blount’s or rickets. As the child grows it is not unusual to note a mild knockknee or genu valgum between the ages of three and five, and this generally resolves itself by the time the child reaches eight years old. Radiographic measurements can be taken to record the angle of the femur and determine the contribution to knee position in the frontal plane. Although indirect, measuring separation of the knees (for genu varum) or separation of the ankles (for genu valgum) is a simple clinical method to follow the progress of the condition. Sustained genu valgum results in persistent pronation of the vulnerable, developing foot, and it can have long term consequences. Similarly, genu varum places a compensating everting force on the subtalar joint of the young child.
Malleolar and Calcaneal Position
At birth there is usually little or no rotation of the tibia relative to the fibula and the lack of axial rotation inclines the foot internally relative to the leg. Gradually the tibia advances relative to the fibula, and the measured angle of malleolar position will reach approximately 14 degrees in adulthood. Soft tissue structures may also contribute to deformity. If the tibia fails to advance there may be a noted adducted gait and resulting compensatory changes in foot pronation.
The foot of a newborn encased in fatty tissue is bulbous, and upon weight bearing there is the appearance of a pes planus. Usually the calcaneus is everted, but during normal development this eversion reduces by about 1 degree per year. A helpful rule of thumb to calculate acceptable calcaneal eversion in the early years is to subtract the child’s age from seven. For example, a normal four-year-old would have 3 degrees of eversion (as 7 – 4 = 3), and by the age of between seven and eight, the calcaneus should be near vertical (7 – 7 = 0).
Limping
Until age three, when walking, children will maintain a wide stance, low center of gravity, and have a non-propulsive gait. This gradually changes through age seven or eight, when they develop a mature gait pattern similar to an adult. In observing a child walk, it is vital to note any deficiency or exaggeration beyond the norm, particularly an asymmetry. As you watch them walk, observe head position and see that the shoulders and pelvis are level. Obvious tilting may indicate the presence of a serious condition that would need to be addressed immediately. Sometimes there will be a complaint of pain, but this is not always the case. Due to the many possible factors that could contribute to a child limping, the rule is to consider serious disease until proven otherwise. Pediatric orthopedists have developed etiologic tables of the more common conditions causing a limp. They include congenital, vascular, neurologic, metabolic, idiopathic, and traumatic categories. The age of the child can also be helpful in isolating the cause of a gait anomaly. For example, a congenital dislocated hip or neurological disorders should always be considered in young children.
From ages three to seven, trauma or infection of bones and joints can be common as well as other diseases such as Legg-Calvé-Perthes or muscular dystrophy. Normal gait can be affected by pain, neuromuscular abnormality, contractures, and limb-length difference. Other specific disorders such as scoliosis, arthritis, and knee problems may develop in the adolescent and also need to be considered. Despite the potential serious causes, don’t overlook the obvious. Sometimes a simple plantar wart or an embedded splinter or other foreign body will be the culprit.
The development of the lower limb can be considered as a gradual unwinding as the infant matures and learns to walk. It is a miracle of unfoldment that usually occurs quite naturally through a combination of bone growth, muscle development, and weight bearing ambulation. Understanding the processes and knowing the milestones allows us to observe the growing child and remain aware when aspects of his or her development are outside normal ranges. Detecting and correcting potential problems in children allows us to do some of our best work guiding proper development. This article is simply an introduction to a rich and rewarding topic.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via email at seamus@hersco.com or by visiting www.hersco.com.
References are available at www.opedge.com.

