Patients with rheumatoid arthritis often benefit from semi-rigid functional orthotics. It is quite unorthodox to begin a discussion with a conclusion, but I did not want this important insight to be lost in the body of the article. Now that we have a conclusion, let us look at some of the ideas and evidence that support this statement.
Arthritis is a debilitating and wide-ranging disease characterized by joint inflammation, pain, and loss of function. It affects more than 40 million Americans, and there are more than 100 different forms of the disease. The two most common types are osteoarthritis (OA) and rheumatoid arthritis (RA).
Osteoarthritis is the most prevalent form of arthritis, affecting more than 50 percent of all sufferers. In the simplest terms, OA is a chronic condition characterized by the breakdown of joint cartilage resulting in pain, stiffness, and use limitations. OA can develop from factors such as age, obesity, injury, overuse, or genetics, and is sometimes referred to as “wear-and-tear” arthritis. It may be local to a single joint or across many sites and is most commonly seen at the knees, hips, ankles, and hands.
For more information about the many varieties of arthritis, visit these websites:
Rheumatoid arthritis is an entirely different condition. RA is a painful systemic disease that attacks all of the body’s joints, resulting in inflammation and swelling, cartilage and bone breakdown, and joint dislocation. This sequence leads to skeletal loss of shape and alignment, pain, and loss of movement. It affects women at least two times more frequently than men. The exact cause of this autoimmune disease is unknown although it is thought that genetics and environment play a role. Typically, symptoms of RA will appear in patients between the ages of 20 and 45, but the condition is notoriously difficult to diagnose. This turns out to be a great disadvantage to the patient, the physician, and the orthotist, as early intervention can delay the onset of joint destruction and biomechanical limitations.
Medical diagnosis is usually made with physical examination, x-rays (confirming joint erosion), and blood work, although the patient’s primary response is to pain. Rheumatologists can treat RA with an array of medications, physical and occupational therapies, orthotic supports, and strength and movement programs.
The primary goals of orthotists and pedorthists in treating patients with RA are to reduce pain, prevent or limit further joint destruction, and keep the patient active and functioning. Limiting weight gain reduces the potential wear on joints. In short, where possible, we want to maintain or improve the patient’s quality of life. There is evidence of increased depression and fatigue among RA sufferers, so anything we can do to help keep these patients active and engaged can help.
Accommodative Foot Orthotics
The vast majority of RA patients will develop foot pathology, and in over one third of the cases, the foot will be the initial site of involvement. Typically, patients will present with combinations of metatarsalgia, rearfoot valgus, arch collapse, or first-MPJ changes. Due to the painful nature of the disease and the collapsed foot structure, the conventional approach has been to prescribe accommodative orthotics. These devices seek to provide cushioning for the foot, incorporating depressions and reliefs at boney prominences such as a dropped met head or a protruding navicular.
Functional Foot Orthotics for Rheumatoid Arthritis
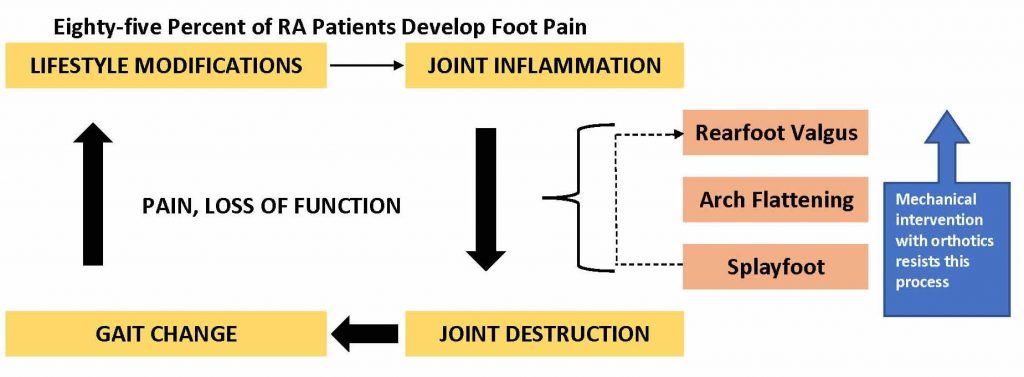
Research over the last two decades has looked at the effect of providing semi-rigid thermoplastic foot orthotics to RA patients. There is now considerable evidence to suggest that patients do quite well in functional foot orthotics. Although soft orthotics will help lessen impact and relieve pressure on the foot, firm, functional orthotics can hold and stabilize the foot and prevent further joint destruction. There appears to be a progression in the foot pathology: rearfoot valgus, arch flattening, splayfoot, and lesser digit deformities. It is thought that limiting movement away from the end of range of motion (ROM) will better preserve the foot structures. When fabricating functional foot orthotics for RA patients, do not attempt to over-correct the foot: build a firm plate to maintain an optimum position.
For more information about the research on the effects of providing semi-rigid thermoplastic foot orthotics to RA patients, see “A Guide to Pathology Specific Orthoses for RA,” by Cherri Choate, DPM, Podiatry Today, April 2007.
The use of semi-rigid functional devices addresses several concerns in the RA foot. First, the rearfoot will be stabilized and the orthotic will resist excessive calcaneal valgus. Deep heel cups, intrinsic and extrinsic posting, and cast skives will enhance the effect. Second, midfoot collapse can be controlled. Requesting a wide medial trim line will capture more of the collapsing arch. A wider foot plate will only work if the patient has a shoe with a sufficiently wide shank to accept the shell. If the patient has a dropped navicular, it may be necessary to include a depression in the shell to avoid pain and irritation. A wide plate also increases the total contact/surface area, thus redistributing pressure.
A frequent site of pain is at the met heads. In general, good support at the arch can relieve some of the pain at sensitive met heads by transferring it back to the arch. You can also request met pads, met bars, or drops for the device. Degradation of the first MPJ can lead to hallux rigidus. This can be addressed with rigid Morton’s extensions or shoe modifications (discussed below). Finally, the use of full-length shock-absorbing top covers such as Spenco, urethanes (PPT or Poron), or thin (3mm) EVAs will provide the cushioning that most wearers seek.
Pedorthics and Rheumatoid Arthritis
Patients with arthritis can benefit significantly from pedorthic services. The choice of appropriate shoes and the modification of footwear can greatly improve quality of life. The certified pedorthist can provide shoes that are a comfortable and stable platform to keep RA patients active, whether the shoes are used alone or in conjunction with custom foot orthotics. Maintaining ROM at the foot and ankle enhances kinematics further up the biomechanical chain.
Primary objectives for the pedorthist include: (1) providing pain relief and shock absorption; (2) providing support and stability; (3) accommodating the abnormalities of foot shape such as severe hallux valgus and hammertoes; (4) controlling excessive motion that might lead to further joint erosion.
Because early intervention is beneficial in delaying the onset of the most debilitating aspects of foot pathology, all RA patients should wear comfortable, extra-depth shoes that fit well. Shoes with a firm counter, a stiff midsole, a removable inlay, and a mild rocker provide the best foundation. They should also be roomy enough to accommodate custom foot orthotics and not irritate mild hammertoes or bunions. Whether the shoe is custom or off-the-shelf, the orthotist may consider including the following useful modifications:
Rigid soles: Very often, the primary site of pain is at the metatarsal heads. Excessive flexion causes discomfort, and this in turn can lead to the patient developing a compensatory gait. A variety of stiffeners can be added to the shoe to provide a more rigid sole.
Rocker soles: Another solution for reducing flexion is the addition of a rocker sole. There are many styles of rocker and their effect is to allow a smoother gait while reducing flexion at critical joint locations. For example, patients with limited ankle motion may benefit from a “CAM” type of rocker.
Flares: Instability of the rearfoot or forefoot can be controlled using combinations of medial and lateral flares. The addition of extra material to the outsole of a shoe provides a wider base that will resist eversion or inversion. In extreme cases, the flare material can be built up along the upper of the shoe.
Wedges: The addition of a varus or valgus wedge onto the outsole can be helpful in accommodating a fixed deformity. It is also useful for stabilizing a flexible foot, much like a post on a custom foot orthotic.
Solid-ankle cushion-heels (SACH) heels: SACH heels are a good option for reducing impact during the early phase of gait. SACH heels are wedges of softer and more compressible material that can be inserted into the midsole, under the heel.
We began the discussion with a conclusion, so it is only fitting that we end with a good opening. Rheumatoid arthritis is a prevalent and debilitating condition. Orthotists and pedorthists can have a significant impact in treating and retarding the biomechanical aspects of this disease. Early detection and treatment offers the best opportunity to maintain good quality of life for RA patients.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York, New York. He can be contacted at seamus@hersco.com or by visiting hersco.com.