The statistics about diabetes are staggering. In 2017, the Centers for Disease Control and Prevention estimated there were more than 30 million adults in the United States with diabetes, and close to 24 per- cent of that number were not aware or did not report the condition (https://www.cdc.gov/diabetes/php/data-research/methods.html). This equates to almost 10 percent of the US population living with the disease, and that rises to over 25 percent for the population of adults age 65 or older. Beyond these sobering numbers, it is estimated that based on fasting glucose or A1C levels, an alarming one-third of US adults had pre-diabetes in 2015.
Because medical costs for people with diabetes are more than twice as high as for those without, the direct economic impact and the burden on the healthcare system is and will continue to be immense. In addition to the financial toll, as the disease progresses it can directly affect a patient’s ability to ambulate and quality of life. As O&P professionals, we recognize the diabetic foot is one of the most serious and costly ramifications of the disease. The good news is the complications of diabetes are far less common and less severe in people who have well-controlled blood glucose. Orthotists, pedorthists, and podiatrists are often on the front line of the fight to prevent or delay the onset of pedal problems. It is frequently up to us to recognize the early warning signs, generate a sense of urgency, and educate patients and their healthcare teams.
The Diabetic Foot
In diabetic foot disease, diabetic peripheral neuropathy is the primary risk factor for the development of foot ulcers. Neuropathy in general is nerve disease or damage. Diabetic neuropathy is nerve damage that develops as a result of elevated blood glucose levels. This is particularly destructive to the fine peripheral nerves of the foot and hand. Loss of sensation coupled with the repetitive stress and load of walking means that the effects of diabetes frequently involve the feet first. Robbed of the gift of pain, patients can literally give themselves a foot ulcer just by going about the normal activities of a day.
What sometimes makes the diagnosis difficult is that up to half of patients may not present with any symptom. Some will complain of pain, which is typically worse at night and at rest, yet others will be pain-free despite having a foot ulcer.
Nerve Damage
The diagnosis of neuropathy covers three distinct nerve types: sensory, motor, and autonomic. Sensory neuropathy leads to a loss of the protective sensation in the foot, making the feet vulnerable to injury. The sensory nerves, when healthy, provide information on pain, temperature, touch, vibration, and sense of joint position.
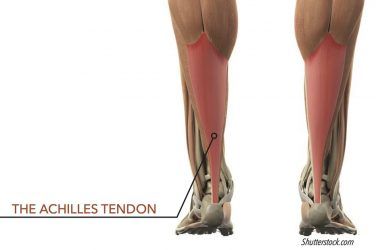
Motor nerves help regulate the intrinsic muscles of the foot. Disrupting them can lead to atrophy, muscle imbalance, and joint instability. Motor neuropathic changes can manifest as involuntary muscle contracture. If this results in a change of foot shape or creates a more rigid foot, it can lead to areas of localized pressure creating conditions for ulceration. The effect on the feet can be seen as a clawing of the digits, hammer toes, and increased pressure on the plantarflexed metatarsal heads. When there is an accompanying anterior migration of the plantar fat pads, less ability to absorb shock, and no perception of pain (due to the sensory neuropathy), repeated cycles of stress will lead to breakdown of the skin. This cycle of events and the resultant foot shape is referred to as the intrinsic minus foot.
In relation to the feet, autonomic neuropathy impairs vasoregulation,
the dilation and contraction of blood vessels. This can lead to dry, friable skin prone to stiffness and cracking. Stiff skin is less accommodating to friction and may cause hyper-keratotic lesions to develop. Alternately, excessive perspiration leads to increased moisture and the potential for fungal infection.
Part of the challenge in treating diabetes is that complications develop gradually. This frequently creates a false sense of complacency with patients, and they feel no immediate reason to change diet or exercise habits. This is a dangerous assumption as neuropathy is irreversible. Initially, the sense of vibration is lost. As sensation diminishes, the effects of motor neuropathy and position sense also begin to take hold. When the small muscles of the foot become affected, creating weakness, atrophy, and imbalance, the biomechanics change. Further progression can limit joint mobility and the ability to walk, which can set off a cycle of less exercise leading to difficulty regulating weight and blood sugars. Once pain and temperature sensation are lost, the foot is in jeopardy and without constant vigilance an ulcer is almost inevitable.
Testing and Screening for Neuropathy
In response to the critical need for the prevention of foot ulcers, the International Diabetes Federation (IDF) has created an extensive archive of material and references for healthcare practitioners.1 Their Diabetic Foot Screening Pocket Chart is an excellent guide to quickly evaluate and determine a patient’s risk category (Table 1). This includes a protocol for follow-up and an initial treatment plan based on the staging.
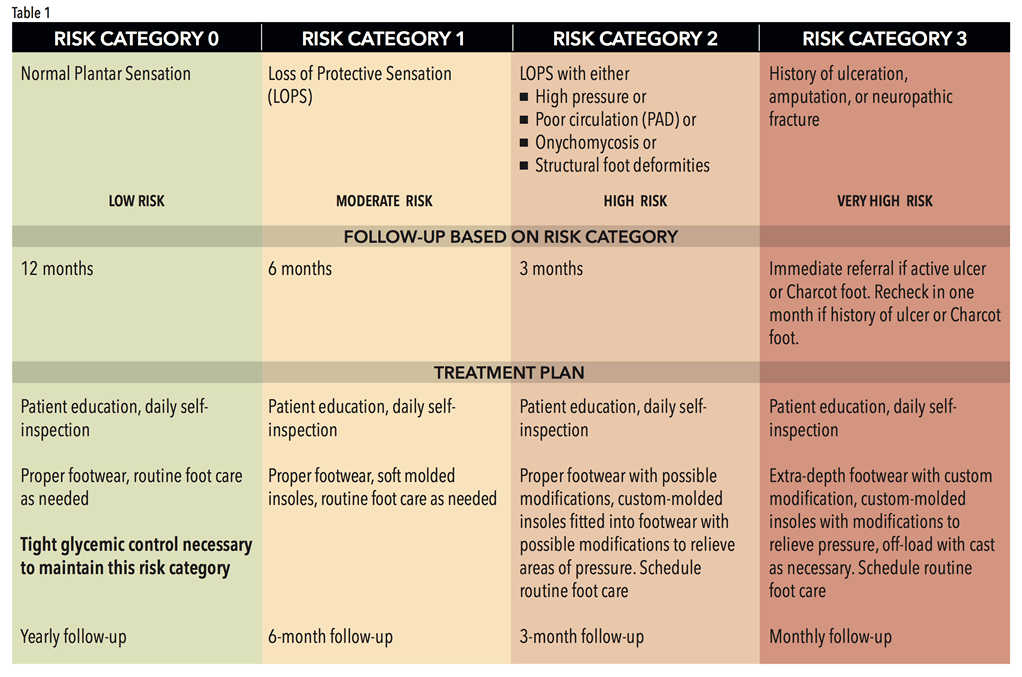
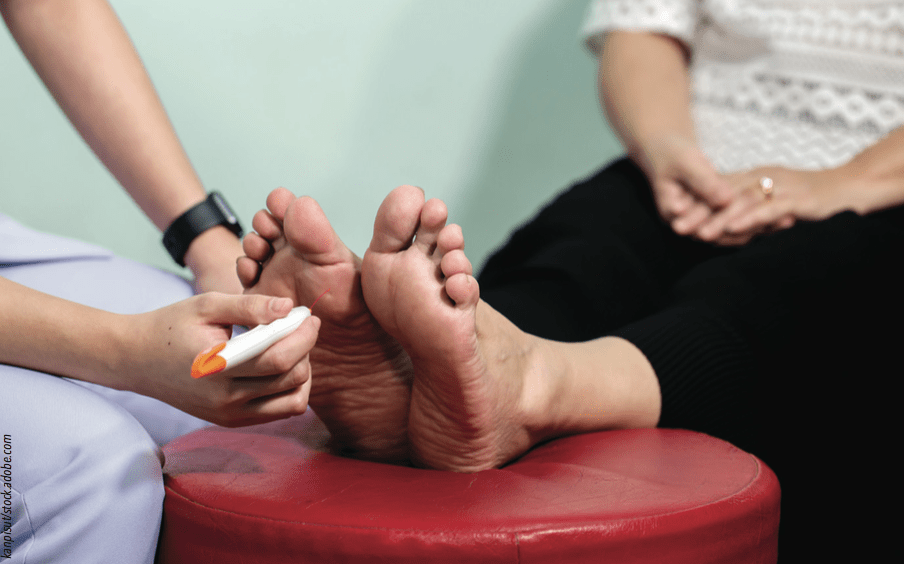
The following foot screening is recommended for diabetic patients at risk for peripheral neuropathy:
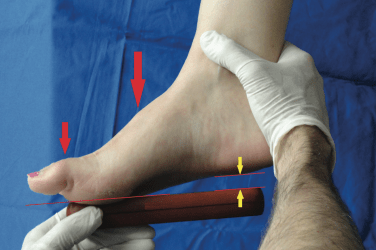
- Record touch pressure sensation using the Semmes-Weinstein monofilament.
- Test for loss of sense of vibration using a 128Hz tuning fork.
- Measure vibration perception threshold.
- Test temperature sensation by applying hot and cold surfaces to the skin on the dorsum of the foot. If temperature sensation is lost, then pain sensation is also usually lost.
- Assess the patient’s sensation of pain. Neuralgia is a common manifestation of neuropathy, which may include tingling, burning, aching, shooting, or stabbing pain.
- Check for ankle reflex. Test extrinsic muscle strength by having the patient flex and extend their ankle, and their toes. Also have them heel walk.
Foot Care and Footwear
Once patients have an established diagnosis of diabetes and their risk category is determined, it is essential that they adhere to their prescribed follow-up plan. There are several complicating factors that appear deceptively minor but put the feet of people with diabetes at great danger. Patients should be encouraged to adopt a program of regular foot care including clipping toenails, removal of corns and calluses, and daily washing and self-inspection. These steps prevent the buildup of potential pressure spots and keep the feet free of fungal infection. Although onychomychosis occurs in 2-13 percent of the general population, it is usually considered only a nuisance that discolors and thickens toenails. However, in people with diabetes, the incidence rises to approximately 35 percent. As the nail pulls away from the nail bed, it opens pathways for bacterial and fungal infections to enter, which increases the risk of ulceration and gangrene by threefold.
Appropriate footwear is important for people with diabetes, especially if they are insensate. Good shoes must be well fitting with sufficient space in the front—both the length of the shoe and the height of the toe box. It is not unusual for a patient to have slightly different left-to-right foot measurements, so it is important to measure both feet and protect the longest toes. The toes should be covered to protect the digits and the shoe should have a sufficiently stabilizing heel counter. The inside should be seamless, particularly in the forefoot. Extra-depth shoes with removable inlays allow the practitioner to modify the existing insole, redistributing pressure. Depth construction will also accommodate an orthotic if one is prescribed. Patients should be advised to change their shoes daily, not wearing the same pair on consecutive days. This allows shoes to air out, drying any perspiration that may have accumulated, creating a less attractive environment for bacteria and fungus. Recognizing these benefits, the Medicare Therapeutic Shoe Bill was enacted by Congress to provide proper footwear and inserts for people with diabetes who qualify under Medicare Part B. Overall, the program has been successful in preventing lower-limb ulcers, amputations, and other complications for many people who suffer from the disease.

Foot Orthotics
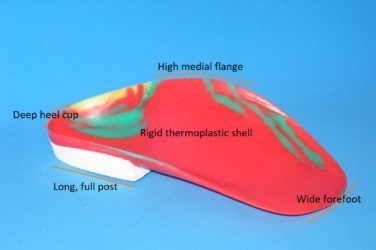
Full-foot, custom-molded orthotics can be made with reliefs for areas of high pressure. The right choice of materials will provide cushioning, reduce shearing friction, and protect the skin from breakdown. They will also help control foot position and reduce excessive pronation. Accommodative foot orthotics are made from a variety of materials such as EVAs and corks. Prescribing deep heel cups and flanges can help cradle the foot and provide stability. Foot orthotics with soft top covers protect the skin. Plastazote is often the first choice of material, but it does need to be refurbished frequently before it wears down excessively.
Complications
As part of the advancing disease process, diabetes can lead to the development of further complications. For example, peripheral artery disease (PAD), the narrowing of arteries or blood vessels, is twice as prevalent in people with diabetes and is a major cause of amputation. The reduced blood flow from PAD not only lowers a patient’s healing capacity but also inhibits the delivery of antibiotics to affected sites. Therefore the development of an ulcer or any foot infection is a cause for major concern. Having studied the causal pathways for diabetic foot ulceration, the IDF recommends asking whether the patient has any of the following conditions:
- Peripheral neuropathy
- A foot deformity (boney prominence, hammer toe, corn, or callus)
- A history of diabetic foot pathology
If a patient has any of these, he or she is at a much greater risk of ulceration and potentially amputation.
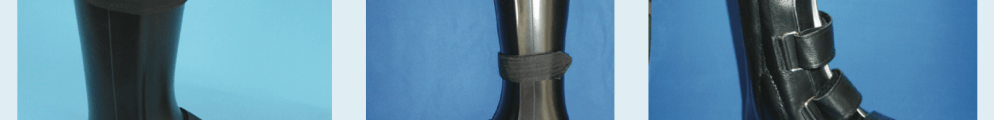
Finally, practitioners need to be aware of the potential for developing Charcot foot (Charcot osteoarthropathy). This is a serious condition brought on by advanced neuropathy. The loss of sensation in the foot creates conditions in which the foot shape and integrity is completely lost, bones easily fracture, and the foot then remolds. The main treatment objective is to protect the Charcot foot in its initial stages so when the active stage is over, the foot is stable and capable of supporting the body without resulting in areas of high pressure. It can take months to resolve an occurrence of Charcot and may require surgeries, serial casting, AFOs, and eventually custom orthotics and shoes.
Conclusion
Foot health is key to overall health. Keeping patients on their feet, walking, and mobile is fundamental to preventing the progression of many lifestyle-related diseases. Simply by walking, people with diabetes will have improved blood glucose control and weight management. People will not walk if they have pain, balance issues, or fear doing more damage to their feet.
Since it is estimated that 80 percent of the cost of treating the diabetic foot occurs in risk category three, our goal is to keep our patients upright and moving safely for as long as possible. With the correct treatment and recommended lifestyle changes, many people with diabetes are able to prevent or delay the onset of complications, avoiding serious consequences to their health and well-being. As foot health professionals we must be vigilant for early detection, advocates for early treatment, and a voice for education.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
Reference
1. The International Diabetes Federation Clinical Practice Recommendations on the Diabetic Foot 2017. A guide for health care professionals: International Diabetes Federation https://idf.org/media/uploads/2023/05/attachments-61.pdf
Portions of this article were excerpted with permission of the International Diabetes Federation (www.idf.org).