One aspect of the orthotic industry that can often be overwhelming and confusing to newcomers is the range of materials available. In addition to the many different types and varieties of actual materials, there are also a myriad of trade names to contend with.
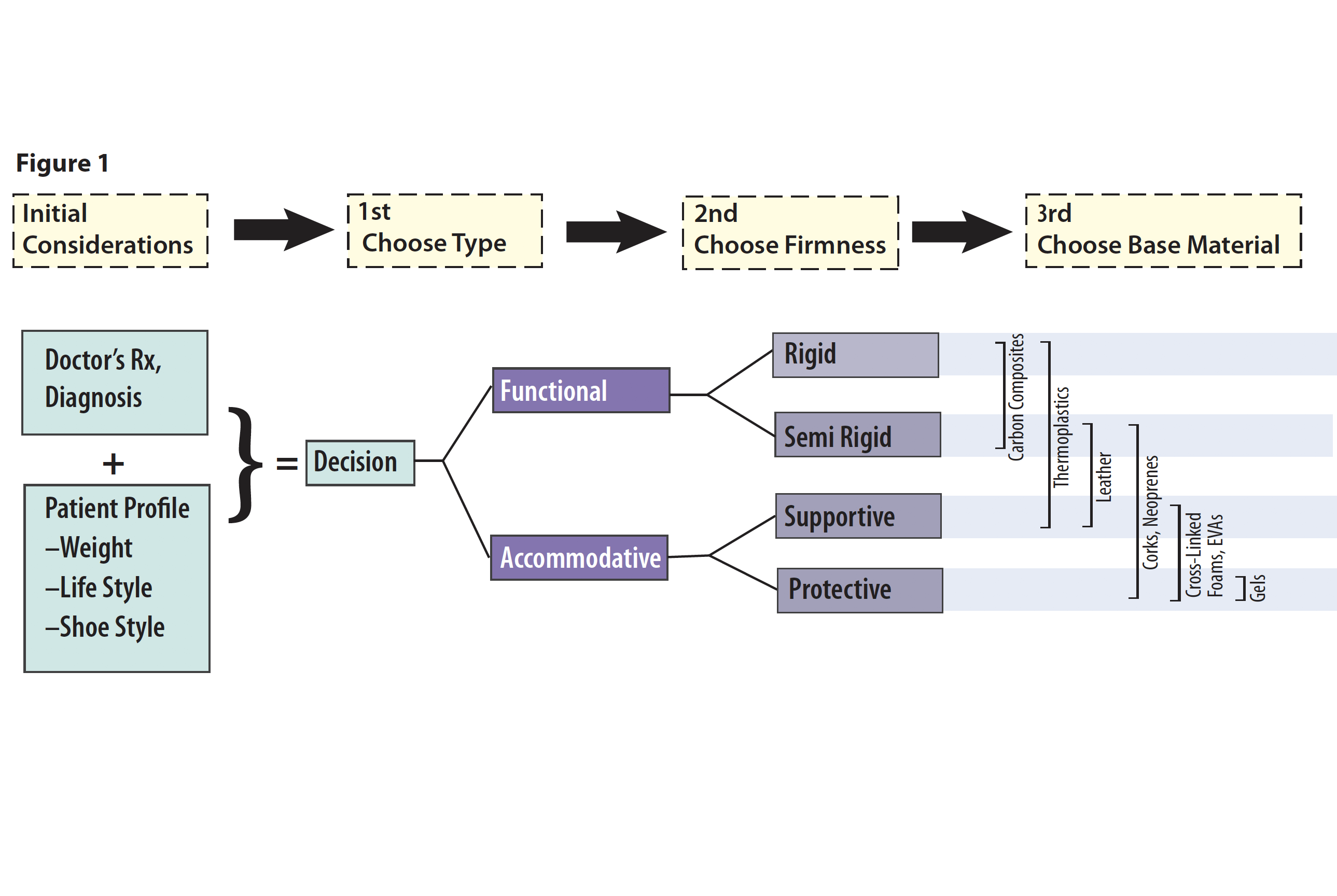
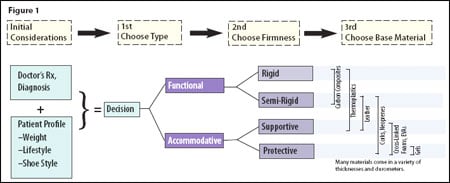
Before looking at some of the more popular materials used for foot orthotics, let us first examine some of the design criteria that go into their development. How you design the orthotic will strongly influence the materials chosen. In essence, the design is a series of decisions and selections that leads to the final product.
Usually there are several disparate objectives that need to be met in order to realize the optimum outcome. We demonstrate our value and worth as a profession in skillfully balancing these competing demands. First, we must follow the physician’s prescription, or involve the physician in a conversation to help develop the best device possible. Second, we want to heal the patient. This must be done as we consider the patient’s specific diagnosis and the relevant biomechanics. Thirdly, we should always aim to satisfy the customer while not compromising our standards of care. Unfortunately many of us know the challenges patients can present: hoping for a low-cost and speedy miracle that will not take up any room in the shoe. Other considerations can include longevity of the device and speed of delivery.
Initial Considerations
Over the years I have developed a flowchart to guide me through the design process (figure 1). Although the first step has little to do with a physician’s prescription or biomechanical exam, the entire success of the orthotic may well depend on the patient’s weight, shoe style, and lifestyle.
The patient’s weight is a critical piece of information that a lab must have if it is to make a correct material choice. For example, 4mm Subortholen® may be rigid for a lightweight 135-pound athlete, but it will be flimsy for a 250-pound construction worker with a size 13 shoe.
Shoe Styles and Orthotic Type
The shoe styles that a person wears will influence the type of orthotic that will work best for him or her. If the patient is a professional and experiences general foot pain on a daily basis, then the orthotics will need to fit dressier shoes. Likewise, if the patient is very active and is strictly using them during training, then the orthotic may only need to fit into a sneaker. Well-fitting shoes with a firm counter, a sensible heel height (1/2 inch to 1 inch), and a removable inlay will help to ensure the proper use and success of the orthotics. Frequently it is necessary to educate the patient about the combined benefits of orthotics plus good shoes.
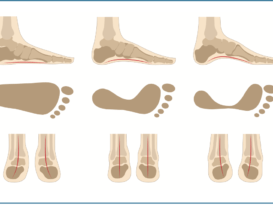
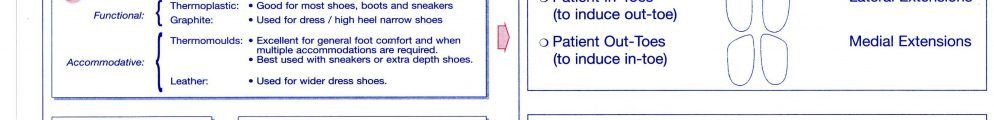
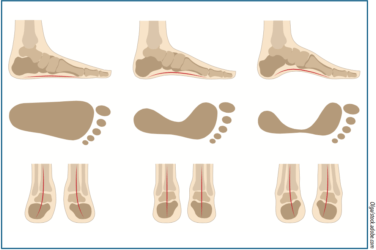
In general, foot orthotics fall into one of two broad categories: functional or accommodative. Functional orthotics seek to control the subtalar joint (STJ) and foot biomechanics, while accommodative orthotics minimize changes to foot function while providing relief and/or protection to specific areas of the foot.
Functional foot orthotics are usually made from thinner, firmer materials. Subortholen, polypropylene, copolymer, and the carbon graphite composites are all good choices for functional devices. Usually they will incorporate a deep heel cup and a good medial longitudinal arch. Among other diagnoses, functional devices are used to treat pronation, plantar fasciitis, and heel spur syndrome.
Accommodative devices tend to be made from less rigid materials such as EVAs, Thermocorks®, Neoprene, Plastazote®, etc. Although a little more bulky, they are usually molded to the entire plantar surface of the foot, providing comfort. In general, accommodative orthotics are a good choice for patients with diabetes, early Charcot joint disease, or any form of neuropathy. In addition, they are often the better choice for patients who present with a rigid foot structure or limited range of motion, e.g. cavus foot type, clubfoot, or post-polio syndrome.
Base Material
Knowing the type of device required, you can now choose the most suitable base material for its manufacture. The flowchart shows that there is overlap across the categories. The final choice may depend on practitioner preference, material availability, or a patient’s previous experience. There is a brief description of the major material groups used for the orthotic base in table 1.
This is a broad sketch of base material choices for foot orthotic manufacture. There are even more options when it comes to padding, cushions, and top covers-foams, gels, and laminates to name just a few. In addition, recent technology has introduced the metallic elements silver and copper into top cover and sock materials. Knowledge of the full array of material choices allows the practitioner to design and develop the ideal orthotic for each patient’s needs.
Table 1: Orthotic Base MaterialsThermoplastics Polypropylene Subortholen Family Acrylic Composite Carbon Fibers Cork Leather Polyethylene Foams Ethyl-vinyl cetates (EVAs), crepes/neoprenes, and more recently silicones are other groups of man-made materials that are ideal for making accommodative foot molds. For a fuller discussion of these materials and their chemistry, please refer to Foot Orthoses and Materials by Bob Schwartz, CPed (Eneslow, New York, New York). |
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.