Medial Tibial Stress Syndrome (MTSS) is a common injury of the lower leg that affects runners, athletes, dancers and other active patient groups. It is an exercise induced overuse injury resulting from weight-bearing activity. The previously used term “shin splints” is a poor, vague descriptor that has essentially been retired from the medical literature. It is important to use the correct terminology describing this syndrome as there are several conditions of the lower leg that present similar symptoms but are distinct diagnoses.
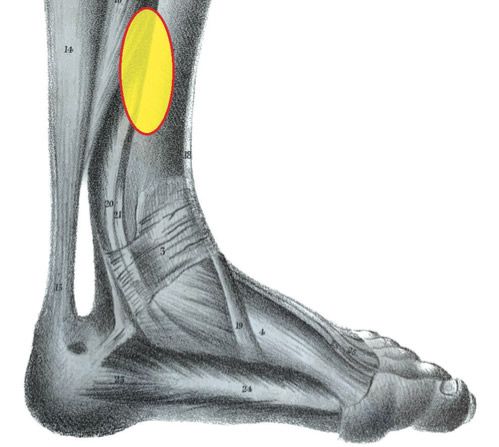
MTSS is often described as intense pain in the lower part of the tibia occurring along the posteromedial border, over a length of at least 5cm (Fig 1). It is a musculoskeletal injury that affects up to 1 in 5 runners, and is also prevalent in military recruits. In its early stage, the pain is exercise induced but may dissipate as the session continues, and it usually resolves with rest. Examination of the leg indicates diffuse pain in the tibia along the medial border, in a region about two-thirds distal. Some researchers view MTSS as part of a continuum that begins with tissue injury but if untreated may eventually lead to reduced bone density and stress-failure. Accordingly, in its later stages the pain may last beyond the period of activity.

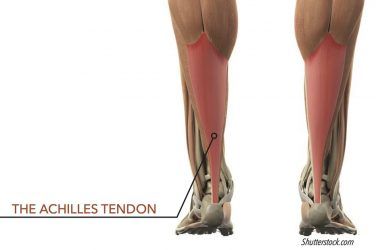
Although the exact causes of MTSS remain under investigation there are currently two suggested mechanisms to explain its etiology. The first proposes MTSS is a fasciopathy. Originally it was thought certain lower leg muscles, when under traction, were being pulled and tearing from their sites of attachment. However, the implicated muscles do not have their origins in the area where the pain was felt. It appears more likely MTSS is a general tibial fasciitis aggravated when the deep posterior muscles of the lower leg are overly active.
The second theory considers MTSS the result of bone overload. Bending stress produces compression on one side of a column and tension on the other. During running the highest bending stress in the tibia occurs right around the distal two thirds region, matching the location of symptoms. Cortical studies reveal patients with MTSS have reduced bone mineral density in this area compared to normal subjects. It is quite possible that both factors, crural fasciitis from the periosteum of the tibia and bone stress, contribute to MTSS.
DIFFERENTIAL DIAGNOSES FOR EXERCISE RELATED LEG PAIN
When patients present with exercise related leg pain there are several possibilities to consider bedsides MTSS. Most likely it will require scans, radiographs and other tests to make the final diagnosis.

Stress Fractures
The symptoms of tibial stress fractures closely mimic MTSS. In the early stages there will be gradual onset of pain with activity, which often subsides with rest. As the condition worsens, the pain does not decrease with rest, persists when the activity is stopped and is even noted in daily activities. Stress fracture pain tends to be more focused and less diffuse than MTSS. There can be swelling, redness and sensitivity to palpation. The “one-leg hop” is a quick clinical test which may help clarify the problem. If the patient can complete 10 single leg hops it is more likely they have MTSS and not a fracture. Stress fractures are confirmed with bone scans.
Compartment Syndrome
Exertional compartment syndrome is another condition that affects the lower leg. If during activity there is an elevation of pressure within the separate muscle compartments, and blood flow is restricted, it can cause pain. Typically, the patient’s exercise begins normally but they experience pain a set time after commencing activity. They will likely complain of stiffness and tightness in the mid-portion of the lower leg, possibly muscle weakness, and sometimes an ache that remains after rest. They may also report some numbness and weakness of the foot and ankle. Diagnosis is made by pressure analysis. A needle is inserted into the lower leg’s compartments and the pressure is recorded using a manometer.
Other conditions that produce similar symptoms include popliteal artery entrapment and tendinopathy. A careful examination and patient history are essential in isolating the cause.
PATIENT PROFILE
Many factors contribute to the development of MTSS. As an activity-induced pathology the primary component is intense exercise. For example, runners of all categories are at risk: new runners and seasoned pros. Both can make training errors such as increasing mileage or intensity too quickly, failing to take important rest days, running on hard surfaces or in the wrong shoes. As with other sports injuries a previous history of MTSS best indicates a likelihood of recurrence. Other potential risk factors include Body Mass Index, age, females and a rigorous training routine.
Lower extremity biomechanics also seems to play a role. Despite no clear explanation for the mechanism of injury there appears to be correlations with foot pronation and external hip rotation. Although unproven, it is not unreasonable to assume that excessive motion associated with foot eversion and tibial rotation places increased strain on the crural fascia.
One measure of the foot’s weight bearing range of motion is the Navicular Drop test. Have the patient stand in Neutral Calcaneal Stance Position and mark the medial prominence of the navicular. Then, with a ruler in place, let the patient drop into Resting Calcaneal Stance Position and note how far the navicular descends. Normal feet demonstrate some lowering of medial arch height, but a navicular drop of more than 8-10mm is generally considered symptomatic. It is believed abnormal mechanics coupled with sudden increases in activity are leading predisposing factors for developing MTSS.
TREATMENT
The first course of treatment for any exercise induced injury is rest. Typically, athletes and active patients are reluctant to interrupt their programs, but they should refrain from intense training for several weeks. As an alternative, they can maintain fitness by working at a reduced % of previous load or cross-train in low impact activities. It is also recommended to avoid hill running. The time and duration of such modifications are patient specific, but in all cases activity should be halted with the commencement of symptoms. Icing has been shown to be provide relief along with other therapies such as ultrasound and electrical stimulation. If it is thought that faulty biomechanics are contributing to the condition a physical therapy program of stretching and strengthening, including core strengthening, may be indicated. Finally, changing running gait technique to encourage a midfoot strike may lessen stress on the tibia.
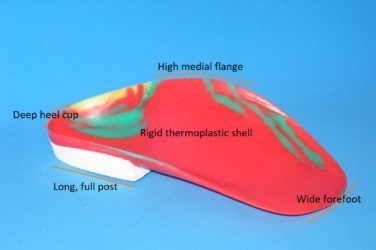
Off-the-shelf or custom orthotics can be prescribed for patients with pronation. Functional foot orthotics with good medial arch support, a deep heel cup and a neutral rearfoot post will help limit excessive pronatory motion. In addition, properly fitting sneakers with a firm heel counter, shock absorbing materials and a heel drop of at least 10mm will help position the foot and protect the leg. The return to full activity should be gradual and monitored closely.
CONCLUSION
MTSS is a repetitive stress injury, the appears to be the result of accumulated micro-damage to the distal tibia. Despite its prevalence the causes are still not fully understood, and there is a dearth of randomized clinical trials supporting effective treatment regimens. Compounding this, several other diagnoses have symptoms that closely match the ache and pain induced by vigorous physical exercise. However, the debilitating effects of MTSS can be countered by modifying the intensity and frequency of activity. Although combinations of rest, physical therapy, shock absorbing footwear and orthotics are known anecdotally to provide benefits, there is no universal cure. Further work needs to be done to isolate the exact causes of this condition, which in time may lead to more well-defined treatment protocols.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
REFERENCES
- Exploring the Mystery of Medial Tibial Stress Syndrome
Doug Richie Jr. DPM Podiatry Today, April 2021 - Exercise Related Leg Pain: More than “Shin Splints”
Mark Reinking PT, PhD Lower Extremity Review, Feb 2011 - Medial tibial stress syndrome: conservative treatment options
R. Michael Galbraith, Mark E. Lavallee
Current Reviews in Musculoskeletal Med. 2009 Sep; 2(3): 127–133