In a broad sense, gait is defined as a manner of walking. It is a pattern of movement involving balance and the coordination of muscles to propel the body forward in a rhythmic and efficient manner. When studying ambulation, it is important to establish clear, well-defined benchmarks of normal human locomotion, which can serve as a baseline for comparison. However, deviations from normal gait are not uncommon, especially in rehabilitation medicine, and there are accepted classifications for pathological gait. Footcare is an important consideration in gait and overall health, as patients with foot pain, balance issues, or insensate feet modify their gait pattern and even their willingness to walk.
Foot Health and Quality of Life
Foot problems and foot pain are prevalent in the general population, and most people seek medical treatment for their feet at some point in their lives (1). Beyond the specific complaint of pain, foot pain has wider consequences that affect a patient’s overall health and well-being. The immediate results of foot pain may include limited ambulation and completion of activities of daily living, but long-term effects may reduce mobility and inhibit social participation. The net outcome can be a decrease in overall health and a reduced quality of life (QoL).
A group of studies in the last decade focused on foot health as it relates to QoL. Although each population differed, the same methodology was used across all four studies, providing a sound basis for comparison. The sample sizes ranged from 115 to 1,647 participants. To evaluate the impact of foot health related to QoL, the groups completed the Foot Health Status Questionnaire (FHSQ). The FHSQ is a validated test with three sections that assess foot-specific and general health-related QoL. Scoring is assigned across the following domains: foot pain, foot function, general foot health, footwear, general health, physical activity, social capacity, and vigor. In each study, the researchers noted statistically significant differences in foot problems relating to QoL. However, the effects of the specific differences and the domains affected varied depending on the study group (Table 1).
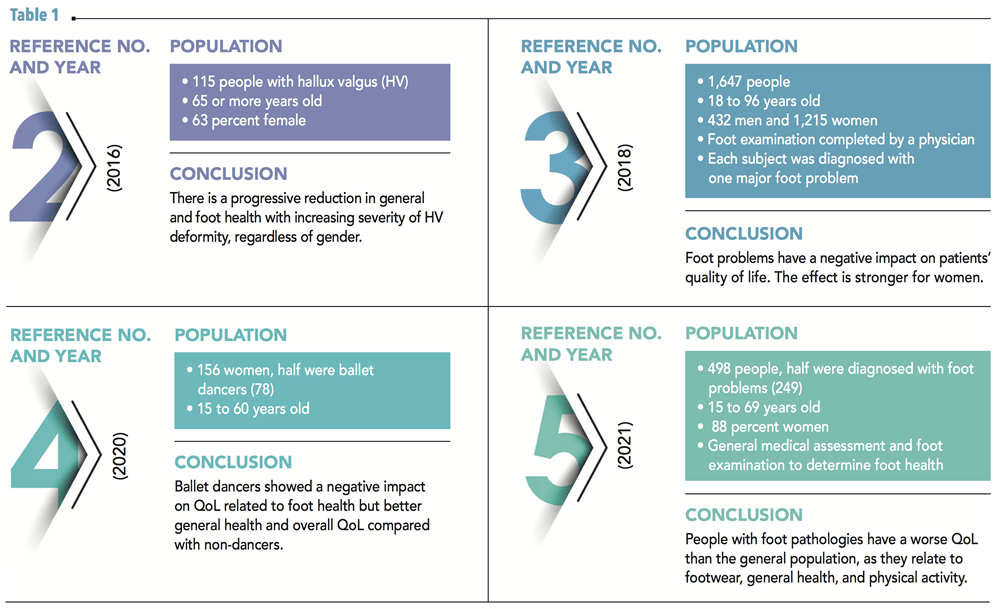
Combined, this group of studies suggests that foot problems negatively impact QoL. This phenomenon appears to be true across different populations and may be more severe for women (3). These results demonstrate the significance of foot health in an individual’s QoL and overall health; accordingly, preventive foot care may help improve these measures.
Mobility Saves Lives
As a profession, one of our aims is to encourage normal, efficient gait in patients, allowing them to remain healthy and active. Several years ago, the Amputee Coalition and the American Orthotic and Prosthetic Association commissioned a study to compare patients who received O&P services against similar patients who did not. They conducted a retrospective analysis of Medicare claims data to determine the extent to which patients who received select O&P services had less healthcare utilization, lower Medicare payments, and/or fewer adverse outcomes. The final research report was titled “Mobility Saves Lives and Money” (6).
The Medicare data showed that patients who receive O&P services have lower or comparable costs than patients who need but do not receive those services. Additionally, patients who receive O&P services experience greater independence than patients who do not, with better or comparable outcomes and Medicare payments.
The results of the analysis suggest that patients who receive O&P services are more likely to obtain the necessary physical therapy and rehabilitation to remain in their communities and avoid facility-based care. Further, the increased physical therapy among O&P users allows patients to become less bed-bound and more independent. Interestingly, this outcome was associated with higher rates of falls and fractures but fewer emergency room and acute care hospital admissions. Although the report focused on the economic impact of O&P devices, it also validated the larger goal of keeping patients active, mobile, and independent.
Gait and Mortality
A well-publicized Australian paper from 2011 examined the correlation between walking speed and mortality. With a little dark humor, the paper was titled “How Fast Does the Grim Reaper Walk?” (7). The stated objective was to determine the speed at which Death walks. The researchers recruited 1,705 men ages 70 years and older, and each was followed up with regularly over a five-year period. The median walking speed of the study population was 0.88m/s. The research determined that those who walked at a speed of 0.82m/s or faster (approximately two miles per hour) were 1.23 times less likely to die than those who walked slower. Within that group, it was also noted those who walked at 1.36m/s (approximately three miles per hour) had no contact with Death, indicating a preferred walking speed for all participants. The researchers speculated that faster speeds are protective against mortality because quick walkers can maintain a safe distance from the Grim Reaper.

This novel paper encouraged several follow-up studies as researchers sought a comprehensive understanding of healthy gait parameters for the elderly. To make the information more applicable to clinical practice, the researchers ascertained how far Death could walk each day (8). Quoting one study, “It is known that distance covered during walk performance tests and weekly walking distance/time are powerful predictors of mortality and future cardiovascular events in selected patients.” (9). The review summarized the relationship between these variables and cardiovascular and all-cause mortality, concluding that fitness and/or ambulatory indexes should be considered a “vital sign” in middle-age and older adults. As healthcare providers, there are many opportunities to promote lifestyle physical activity for patients by recommending pedometers, accelerometers, and smartphone-based health and wellness apps.
Finally, the association between foot health and overall health was underscored in another longitudinal study of 2,110 adults (10). The authors tracked the participants for a mean follow-up of 10.8 years and concluded that within their study group, “taking at least 7,000 steps/day had a 50 percent to 70 percent lower risk of mortality.” Interestingly, step intensity was not associated with mortality regardless of adjustment for step volume. Simply stated, their results suggest that taking at least 7,000 steps/day can extend your life regardless of your walking speed.

Gait and Footcare
Given that walking and movement are vital to overall health, what is the role of foot care? How do foot problems impact gait, and how do they impede ambulation? Faulty mechanics can be the etiology of foot pathology; conversely, foot pathologies can lead to abnormal mechanics. Foot deformity and pain alter gait, affecting speed, efficiency, step length, and duration.
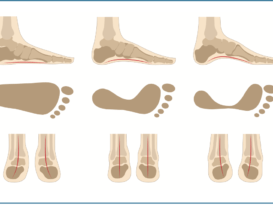
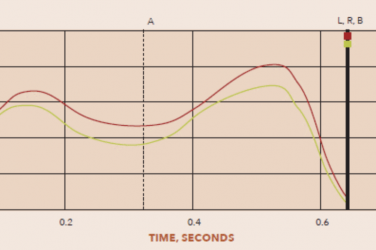
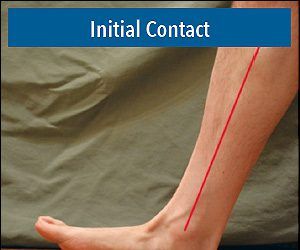
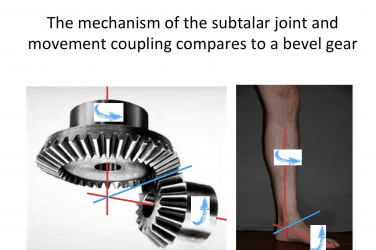
As a mobile adapter, the human body can counterbalance the loads and forces placed on its segments. Compensations occur all the time; they are often short-lived and do not result in injury. However, compensations associated with abnormal structure or function may lead to pathology over the long term. In their seminal text “Normal and Abnormal Function of the Foot,” Root, Orien, and Weed described several intrinsic foot abnormalities that result in pathology. Their list included subtalar varus, forefoot varus, forefoot supinatus, forefoot valgus, and equinus. These common findings are assumed to be the root cause of many pedal problems. Each affects the function of the foot and the timing of pronation and supination in unique ways.
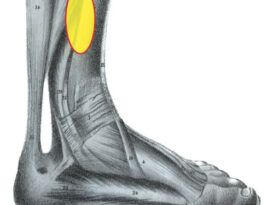
For example, equinus is thought to be present in most of the population. Clinically it can be observed as early heel rise, and you may notice a bouncy-type gait with a pronounced vertical excursion. Compensations for equinus occur dynamically during full weight bearing, and the long-term effects can be devastating. Equinus is believed to be a contributing cause to a wide range of foot problems, including plantar fasciitis/heel pain syndrome, Achilles tendinopathy, calcaneal apophysitis, pes plano valgus, adult acquired flatfoot/posterior tibial tendon dysfunction (PTTD), and forefoot pathologies such as metatarsalgia, hallux valgus, sesamoiditis, and hallux limitus. It is also strongly linked to the breakdown and ulceration of the forefoot in diabetic patients with neuropathy and the destructive effects associated with Charcot neuroarthropathy.
Similarly, functional hallux limitus (FnHL) has a pronounced effect on gait. The inability to pivot on the forefoot in third rocker interrupts the smooth completion of gait. A block at the first metatarsal phalangeal joint (MPJ) directly affects proximal joint motion as the body naturally seeks alternate paths to continue moving forward. One possibility is to abduct and externally rotate the leg, so body weight passes over the side of the foot rather than through its long axis. The result can be excessive pronation or other pathologies remote from the first MPJ, such as knee arthritis and low back pain.
A true block of first MPJ motion also has the effect of interrupting the completion of each step. Every time momentum is halted, energy dissipates into the trunk, contributing to a downward tilt of the head and slouched posture. This block and subsequent lurching may factor into low back pain. To avoid jamming the joint, early toe-off may also occur: the leg gets “lifted” into swing, leading to a shorter stride, which is tiring and less efficient, as natural momentum is lost. Other models posit FnHL as a precursor to hallux rigidus or hallux valgus, which affect gait parameters.
Podiatric medicine is dedicated to the treatment and surgery of disorders of the foot, ankle, and lower limb. Simple procedures such as callus debridement and corn removal can significantly impact a person’s ability and willingness to walk. Routine foot care becomes more important as patients age, plantar fat pads atrophy, and mild bony subluxations become more pronounced and sensitive. Common surgeries such as bunionectomies and hammer toe reductions may appear cosmetic, but realigning important structures of the foot improves ambulation, and walking becomes more comfortable. Combinations of supportive insoles, accommodative padding, physical therapy, proper shoe choice, and pedorthic modifications can restore function, reduce pain, and delay further structural deterioration. In addition, custom foot orthotics and AFOs can be designed to address many intrinsic abnormalities regaining balance and symmetry.

Orthotics and Prosthetics
If movement is essential to life, what is our role as orthotists, prosthetists, and pedorthists? Firstly, we can educate and inform, emphasizing the importance of maintaining active lifestyles to our patients. There is a well-documented higher five-year mortality rate in individuals with diabetes after an amputation (11). While the mortality rate may be related to how sick the individual was before the amputation, caring for them by protecting their insensate feet and preventing foot ulcers in the first place helps distance them from these statistics. Secondly, we get to examine patients and question them regarding their levels of exercise, pain, and discomfort. At times we may notice a change in condition that warrants referral for further medical care and attention. For example, a unilateral warm, swollen edematous foot in a patient with neuropathy is an early sign of Charcot foot, and immediately directing them to a podiatrist may have a major impact on the outcome.
Finally, designing, fabricating, and dispensing orthotics and prosthetics is our direct contribution to supporting patients’ health. These devices are intended to reduce pain and restore function, as well as improve balance, stability, comfort, and confidence. Scores of papers have been written on the efficacy of foot orthotics in treating a wide range of foot, ankle, and knee problems (12-15). Similarly, studies demonstrate the effectiveness of short-hinged AFOs and ankle gauntlets in reducing pain and limiting some of the destruction associated with untreated adult acquired flatfoot and PTTD (16). Whether caring for pediatrics, geriatrics, or any group in between, we have a vital part to play in improving gait and the overall health of the population and, ultimately, increasing the mobility and independence of our patients.
Conclusion
Keeping patients on their feet and mobile is fundamental to preventing the progression of many lifestyle-related diseases. Simply by walking, individuals with diabetes can improve blood glucose control and weight management. Patients will walk less or not at all if they have foot pain, a concern of an injury, or fear of falling. And, below a certain threshold, the slower a patient walks, there is an increased correlation risk of mortality. As O&P professionals, our job is to keep patients up and active, walking steadily, confidently, and pain-free to help them maintain active, high-quality lives as they engage in their communities. Much like a person’s fingerprints or face, each individual’s foot function possesses specific traits, making everyone unique. Studying and understanding human gait, its characteristics and variations, and remaining informed about advances in our field allows us to recommend the very best O&P devices and shoes to help our patients live more fully.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
References
- APMA – Public Opinion Research on Foot Health and Care – Findings from a Survey of 1000 US Adults – September 2010
- Quality of Life Impact Related to Foot Health in a Sample of Older People with Hallux Valgus.
Daniel López López, Lucía Callejo González, Marta Elena Losa Iglesias et al.
Aging and Disease. 2016 Jan 2;7(1):45-52. - Evaluation of foot health related quality of life in individuals with foot problems by gender: a cross-sectional comparative analysis study.
Daniel López-López, Ricardo Becerro-de-Bengoa-Vallejo, Marta Elena Losa-Iglesias et al.
BMJ Open. 2018 Oct 18;8(10):e023980. - Women’s Foot Health-Related Quality of Life in Ballet Dancers and Nondancers.
Daniel López-López, Cristina Fernández-Espiño, Marta Elena Losa-Iglesias et al.
Sports Health. Jul/Aug 2020;12(4):347-351. - Impact of quality of life related to foot problems: a case-control study.
Daniel López-López, Mónica Pérez-Ríos, Alberto Ruano-Ravina et al.
Scientific Reports. 2021 Jul 15;11(1):14515. - Economic value of Orthotic and Prosthetic services among Medicare beneficiaries: A claims-based retrospective cohort study, 2011-2014
Allen Dobson, Kennan Murray, Nikolay Manolov, Joan E DaVanzo
Journal of Neuroengineering and Rehabilitation. 2018 Sep 5;15(Suppl 1):55. - How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over
Fiona F Stanaway, Danijela Gnjidic, Fiona M Blyth et al.
BMJ. 2011 Dec 15;343:d7679. - Brisk and prolonged daily walking is needed to outpace the Grim Reaper
Pierre Abraham, Garry A Tew, Paul S Abraham, Alexis Le Faucheur
BMJ 2012 Jan 17;344:e424. - Reduced walking speed and distance as harbingers of the approaching Grim Reaper
Barry A Franklin, Jenna Brinks, Roger Sacks, Justin Trivax, Harold Friedman
Am J Cardiol. 2015 Jul 15;116(2):313-7 - Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study
Amanda E Paluch, Kelley Pettee Gabriel, Janet E Fulton, et al.
JAMA Network Open 2021 Sep 1;4(9):e2124516. - The Diabetic Foot in a Multidisciplinary Team Setting. Number of Amputations below Ankle Level and Mortality.
T E Wilbek, R B Jansen, B Jørgensen, O L Svendsen
Experimental & Clinical Endocrinology & Diabetes. 2016 Oct;124(9):535-540. - The Effectiveness of Foot Orthotics Part 1: The O&P Edge Jul 2011
- The Effectiveness of Foot Orthotics Part 2: The O&P Edge Sep 2016
- The Effectiveness of Foot Orthotics Part 3: The O&P Edge Mar 2021
- The Effectiveness of Foot Orthotics Part 4: The O&P Edge Jun 2021
- Biomechanics and Orthotic Treatment of the Adult Acquired Flatfoot
Douglas Richie
Clinics in Podiatric Medicine and Surgery. 2020 Jan;37(1):71-89.