Metatarsalgia is a general term used to describe a variety of diagnoses that present as pain in the forefoot. It is considered a symptom and it covers pain occurring at the metatarsal heads, the metatarsophalangeal joints (MPJs) or the soft tissue in that region. Confounding the issue, the pain may be diffuse and difficult to pinpoint. One original paper studied a group of 98 patients who had complaints of pain in the forefoot and isolated 23 separate diagnoses (1).
Classification
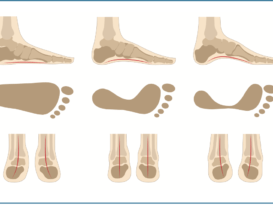
The first broad distinction of the condition is to classify it as primary or secondary. Primary metatarsalgia can be structural or functional in nature – an anatomical abnormality that directly results in an imbalance causing increased pressure under the metatarsal heads. Examples include hallux valgus, hallux rigidus, a plantarflexed metatarsal bone, a hammertoe, or pes cavus. Treatment should be focused on accommodating the uneven weight distribution at the metatarsal heads, mechanically directing force away from the point of pressure.
Secondary metatarsalgia is defined as pain with an origin beyond the metatarsal area itself. For example, conditions such as rheumatoid arthritis, equinus, or a leg length discrepancy can lead to localized pain at the ball of the foot.
In the case of secondary metatarsalgia one needs to address both the symptom and the original cause. Other etiologies include post-surgical or iatrogenic side effects, trauma, osteoarthritis, and neuromuscular diseases that create muscle imbalance.
The Scranton study found that 31 of the 98 patients had two or more mechanical etiologies for primary metatarsalgia, and primary and secondary metatarsalgia often existed together (1). Stated simply, the origin of metatarsalgia can be multifactorial. Effective treatment addresses the area of pain, the function of the foot and, if necessary, the systemic disease.

Keratoses
Hyperkeratosis is a thickening of the skin, and in the feet it is often noted under the metatarsals. This may be due to a plantarflexed metatarsal, an unstable hyper-mobile first ray or an abnormal foot position. The repetitive pressure created by these conditions can result in a buildup of tissue. Hammertoes are frequently a contributing factor as they significantly change the angle of the MPJ and focus pressure on the metatarsal head.
The resulting callus can be categorized based on size. Large diffuse plantar keratoses, or tylomas, lack a discrete core and are typically 1-2cm in diameter. Discrete intractable plantar keratoses or helomas are more localized, deep, and often very painful. They can occur under the larger lateral condyle of the second, third, and fourth metatarsal heads. Plantar keratoses respond well to both debridement and orthotic therapy, both of which work by dispersing pressure.
The Plantar Plate
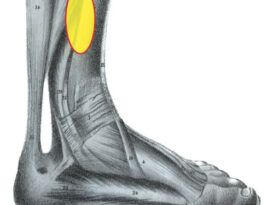
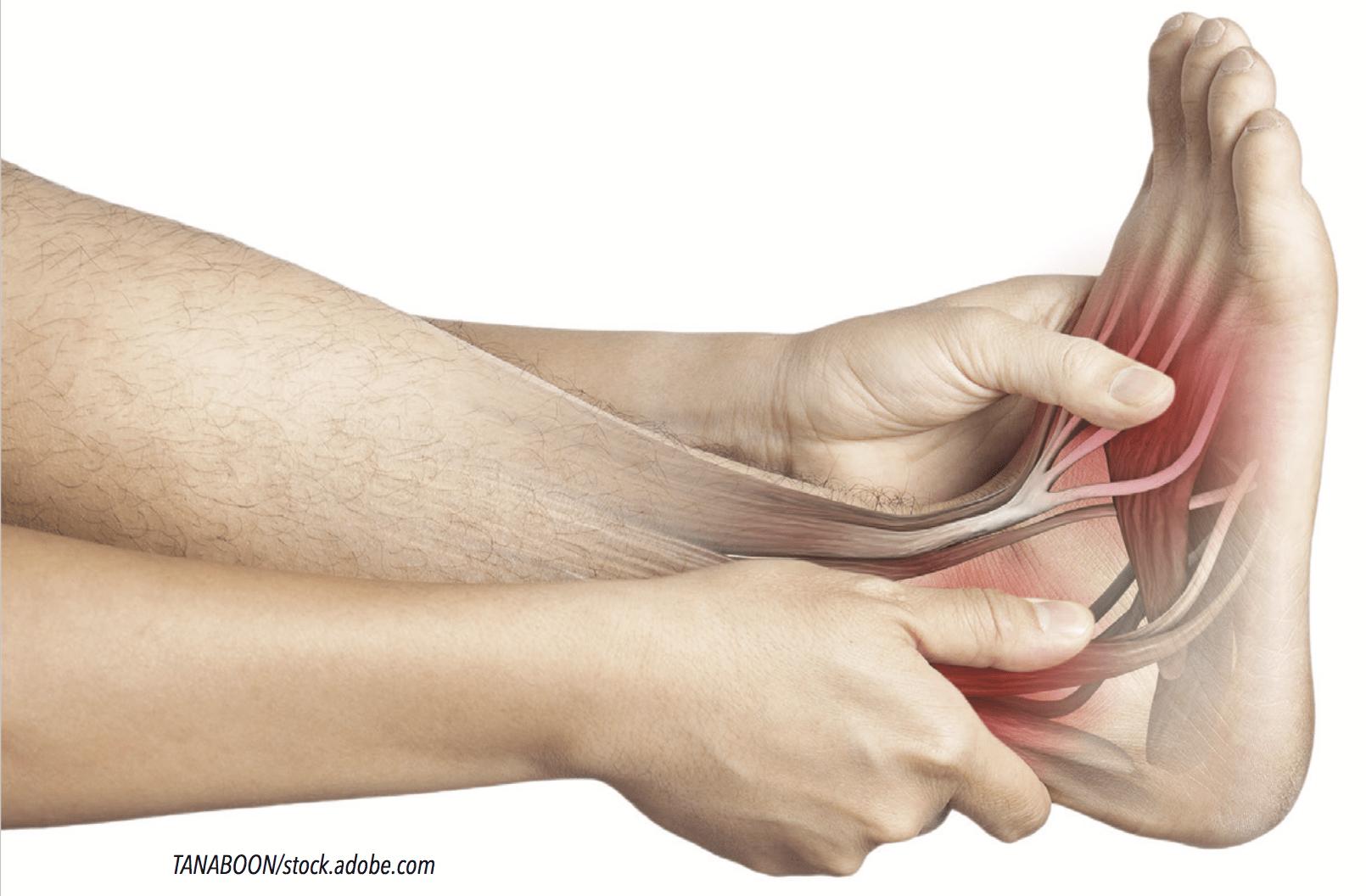
The plantar plate is a fibrocartilaginous structure that lies beneath each of the lesser metatarsal heads. It is a ligament with significant strength that is attached to the plantar fascia at its proximal end. It connects the neck of the metatarsal to the base of the proximal phalanx, and its borders merge with the collateral ligaments of the MPJ. The function of the plantar plate is to keep the toe aligned, preventing medial or lateral drift, hold the digit plantigrade, and allow the metatarsal head to glide over it during gait. It acts like a harness to provide stability for each toe in the transverse and sagittal planes. Because of its attachment and location, it is subject to tensile forces from the plantar fascia and compression by the plantarflexing metatarsal head.
When heel rise occurs the plantar fascia is pulled taut, stretching the plantar plate. Simultaneously the metatarsals plantarflex onto the plate as ground reaction forces reach their second peak late in single limb support. Studies document a much higher incidence of tears in the plantar plate affecting the second metatarsal, probably due to its increased loading in terminal stance. This is especially true if the patient has a relatively shorter first metatarsal bone, or if the first metatarsal lacks stability such as in the case of a bunion deformity.
Clinical tests for an injury to the plantar plate verify the integrity of the digit. The dorsal drawer test is performed by gently lifting the proximal toe away from the metatarsal head. Increased relative motion between the two, when compared to other digits, suggests a tear. Likewise, if dorsiflexion of the MPJ is tolerated but plantarflexion elicits pain, a tear may be suspected. Tears are also recognized by the change in orientation of the digit, and an uneven spacing between two toes is sometimes referred to as the V sign. In addition, it is not unusual to see the toe hammered, and there may also be edema beneath the affected metatarsal head. Originally these complaints were classified as capsulitis or MPJ stress syndrome, but more recent research reveals the critical role of the plantar plate.
Cadaver studies indicate the plantar plate may be damaged more often than is reported, and it appears patients can remain asymptomatic with mild tears. It is important to note the diagnosis can be confused with neuritis, an entrapped or damaged nerve causing aching and burning of the forefoot. However, in the case of a Morton’s neuroma, compression of the forefoot or wearing tight shoes is painful. Ultrasound and MRI are used to make the final determination.
Metatarsal Fractures
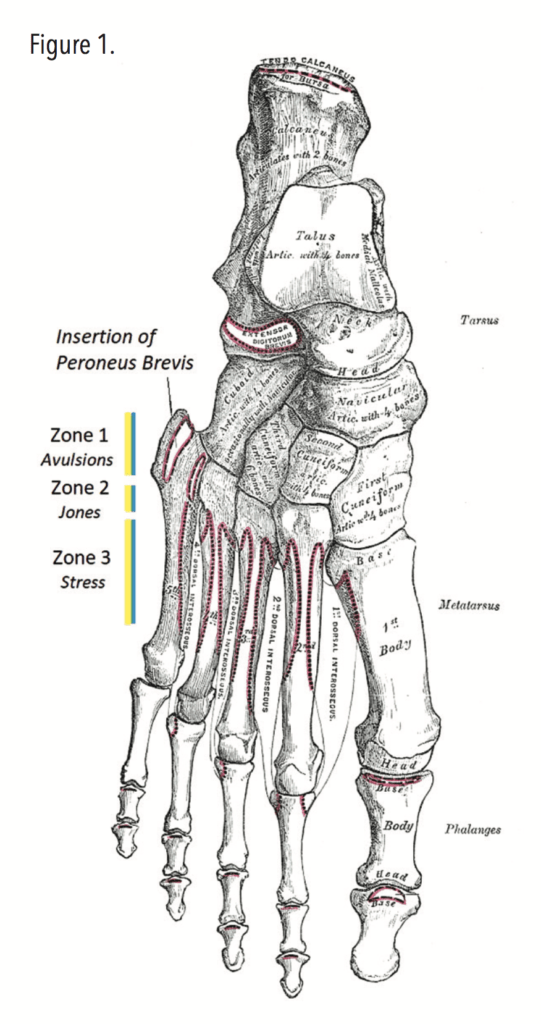
Metatarsal fractures are a distinct pathology separate from metatarsalgia. They are not uncommon and account for approximately 5 percent of all fractures. About two-thirds of metatarsal fractures involve the fifth metatarsal bone. Active, athletic patients are particularly at risk for this type of injury due to overuse and the trauma that occurs from the pivoting and shifting required in sports on the court, in the field, and distance running.
Fifth metatarsal fractures are classified based on the type of injury and its location (2). Zone 1 fractures occur at the proximal end of the bone at the base of the fifth (Figure 1). They are also referred to as avulsion fractures as bone fragments have been forcibly separated or detached from the styloid. Sometimes athletes continue to play with an avulsion fracture, making compensations in their gait, but typically the pain intensifies over time and if ignored may lead to further, more serious symptoms.
Moving distally, Zone 2 or Jones fractures are transverse fractures that occur at the neck or metaphyseal-diaphyseal junction. They often happen due to a single episode where the plantarflexed foot is suddenly inverted or adducted. This is an area of the bone with reduced blood supply, which may delay healing. Zone 3 fractures occurring along the shaft of the fifth metatarsal are more likely to be stress related and may be spiral in nature. They are sometimes referred to as dancer’s fractures due to the occurrence among ballet dancers.
A patient’s biomechanics and foot structure predispose them to fifth metatarsal fractures. It is known that those with a cavus foot type, hind-foot varus, or metatarsal adductus are at greater risk for this injury. The attachment of the peroneus brevis to the fifth metatarsal make it susceptible to fracture if the foot forcibly inverts. Injuries may be acute, occurring from a single traumatic incident such as a sudden ankle sprain, or a more long-standing chronic complaint due to repetitive stress.
Treatment will depend on the severity of the fracture and the time between incident and diagnosis. If the symptoms are mild and there is not a large displacement of the bone, many sports physicians opt to treat Zone 1 and 2 fractures conservatively with rest, limited weight bearing, and protective stiff-soled shoes or a CAM walker. In more serious cases surgical repair is required.
Biomechanics
An appreciation of the underlying biomechanics reveals many reasons why metatarsalgia may occur. Patients exhibiting early heel lift will be at risk for developing metatarsalgia as they prematurely transfer body weight to the forefoot – loading it for a longer period of time. Excessive cyclical pressure can lead to keratoses, plantar plate tears, fat pad atrophy, soft tissue inflammation, and associated pain. Early heel lift occurs when there is an equinus or a leg length discrepancy. First ray function also plays an important role in gait. Hallux valgus, a short first metatarsal, or a hyper-mobile first ray that lacks stiffness can result in weight being transferred laterally, aggravating the lesser metatarsals. Conversely, conditions such as hallux rigidus cause too much weight to be borne by the first ray leading to pathology at the first metatarsal. Careful examination of the patient’s gait and range of motion (ROM) will reveal the cause; from there an appropriate treatment protocol can be developed.
Metatarsal Pads
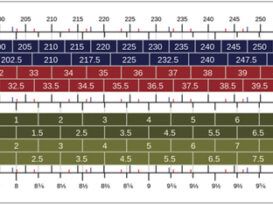
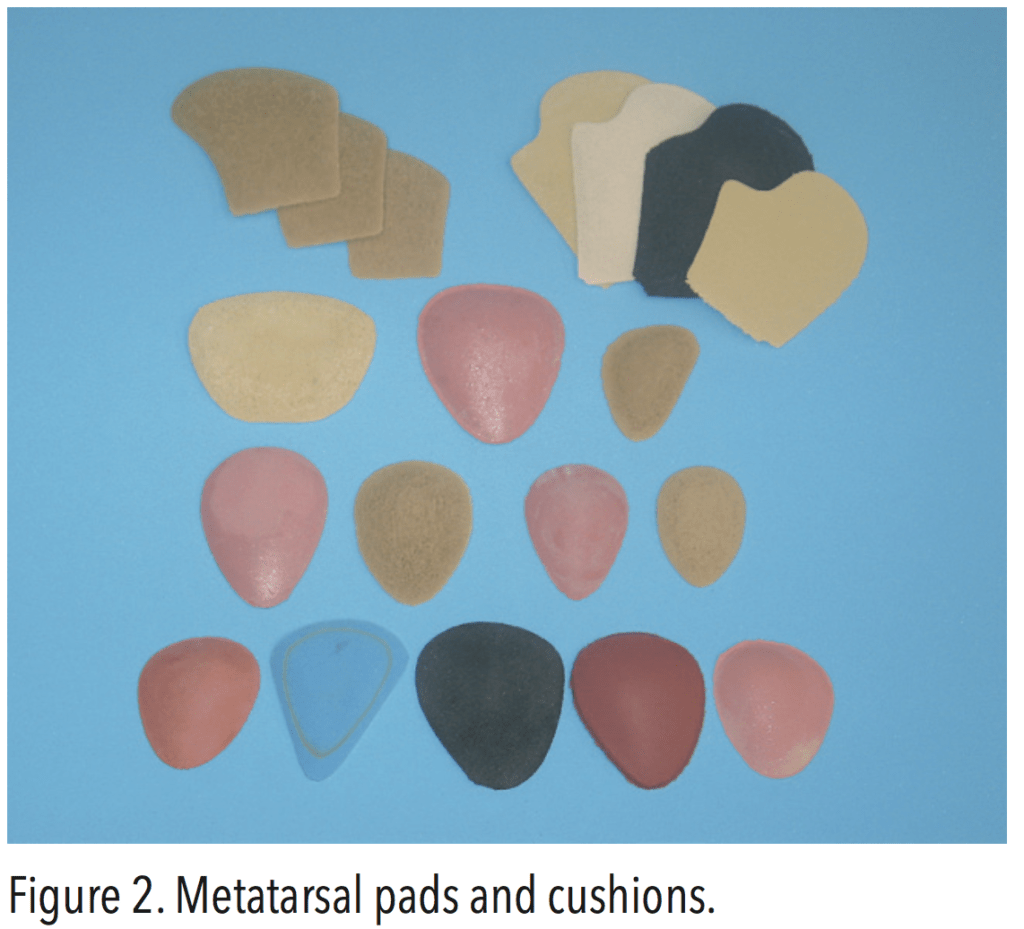
The most common approach to treating metatarsalgia is to off-load the affected area. This can be achieved quite simply through adequate callus debridement and the application of an appropriate metatarsal pad. Metatarsal pads are convex-shaped cushions made from a variety of materials such as sponge rubber, orthopedic rubber, felt, PORON, etc. They come in a range of sizes, shapes, durometers, and heights (Figure 2). The typical pad is designed to sit under the second through fourth metatarsals just proximal to the heads. In the case of first metatarsal pain, sesamoid or dancer’s pads are shaped to provide a deep well or relief for the head of the first metatarsal. The goal is to redistribute pressure away from the point of tenderness and shift it more proximally to the shaft of the metatarsal bone or disperse the load to neighboring metatarsals. In-shoe pressure mapping shows metatarsal pads are quite effective in reducing peak plantar pressures.
A 2007 study investigated the effect of using metatarsal domes with heights of 5mm and 10mm to reduce mean plantar force under the second metatarsal head (3). As part of the study they also moved the pads back (more proximally) from the second metatarsal head in 5mm increments to analyze the effect of proper placement. The research demonstrated that the application of a metatarsal pad significantly decreases the mean force, and placing a metatarsal pad 5mm to 10mm proximal to the metatarsal head provides the maximum reduction in load. Surprisingly, placing the pad even further behind continues to provide almost the same level of relief – although it may not be as comfortable for the wearer. The study also quantified the effect of using a thicker pad. The 10mm pad delivered almost twice the reduction in pressure as noted with the 5mm pad.
Metatarsal pads are frequently placed directly inside shoes. This is an inexpensive, quick, low-volume solution. Practitioners can observe the wear pattern on the insole in well-worn shoes and place the pad in the optimum location. However, fixed pads are not transferrable, so the patient may need pads in many pairs of shoes. Forefoot padding with discrete drops or depressions specific to the site of a prominent metatarsal head also relieve pain.
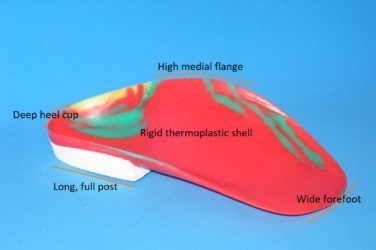
Foot Orthotics
Foot orthotics offer several additional benefits. Firstly, the orthotic shell supports the medial arch and distributes weight across the entire plantar foot and orthotics act to control the dynamic foot, limiting abnormal motion. Secondly, they are transferrable across shoes, so the wearer is not restricted to certain footgear. Thirdly, the metatarsal pad size and location are fully adjustable. Specific prescription requests should include minimal plaster arch fill on the cast, a medial heel skive, and a wide orthotic shell. Where there is excessive pronation, a rearfoot varus extrinsic post will also potentially relieve symptoms in the forefoot.
Other accommodations can augment faulty biomechanics. For instance, with Morton’s syndrome, where the second metatarsal bone is relatively longer, a flexible cork extension under the first will transfer weight medially and help relieve repetitive stress under the head of the second. Note that this only works if there is no restriction in first MPJ motion during weight bearing. Conversely, cut-outs or depressions allow plantar flexed metatarsals to function without having to bear excessive weight. Similarly, the addition of cushioning in the form of soft top covers absorbs impact. Heel lifts are used to correct an imbalance or accommodate equinus. The overall aim of orthotic therapy is to reduce peak plantar pressure beneath the affected met.

Shoe Modifications
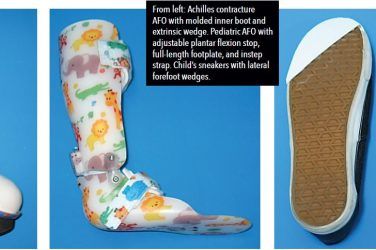
Footwear can be modified in many ways to lessen the pain of metatarsalgia. Leg length discrepancies greater than
1⁄2 in. (12mm) can be addressed by putting appropriate heel and platform lifts directly onto the midsole of the shoe.
If the patient exhibits poor ROM or limited ankle dorsiflexion, a rocker sole can be very beneficial. Rocker bars can be added directly to the outsole to off-load all of the metatarsal heads. If the patient experiences discomfort as a result of flexion at the metatarsal heads, sole stiffeners (either steel shanks or thin carbon plates) can be used to prevent bending. In such cases it is advisable to add a rocker sole to aid in smooth ambulation.
Conclusion
Metatarsalgia is one of the more common complaints of foot pain seen by podiatrists. The causes are diverse, and the resulting pain can be debilitating. If injury is due to dynamic gait, altering the forces and reducing flexion of the MPJ will help alleviate the pain. Careful examination of the symptoms and the correct application of metatarsal pads, reliefs, orthotics, and shoe modifications can provide significant comfort and protection for patients, allowing them to return to active and healthy lifestyles.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
References
1. Scranton, Jr.,P.E.1980. Metatarsalgia: Diagnosis and Treatment. The Journal of Bone and Joint Surgery American Volume 62(5): 723-32.
2. Bowes, J., R. Buckley. 2016. Fifth metatarsal fractures and current treatment. World Journal of Orthopedics 7(12): 793-800.
3. Brodtkorb, T., G. Kogler, A. Arndt. 2008.The influence of metatarsal support height and longitudinal axis position on plantar foot loading. Clinical Biomechanics 23(5):640-7