Toe walking, although not considered part of the normal development of gait, is seen as a common variant that many children go through. Within the general population of toe walkers, the diagnosis of idiopathic toe walking (ITW) remains controversial due to an ongoing debate regarding use of the word idiopathic. In medical terms idiopathic means “of unknown cause,” but some researchers believe this is not the case for toe walking. They argue just because its origins are poorly understood, or currently lack sufficient study, toe walking does not warrant the idiopathic label. Recent research has been looking at a host of factors, such as patient motor sensory deficits, sensitivity to vibration, and a possible genetic link, that may be contributing to this unique gait style. Another term used to describe persistent walking on the balls of the feet by otherwise normally developing children is habitual toe walking.
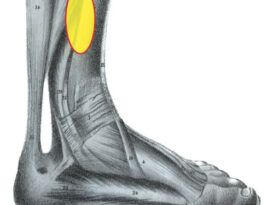
There are several known etiologies of toe walking that are well documented. For example, toe walking is one possible compensation for an Achilles contracture. Likewise, an abnormal soleus or defects of the central nervous system that result in equinus may cause a child to walk without heel contact. Toe walking associated with pathologies such as cerebral palsy (CP), muscular dystrophy, and autism is more clearly understood, but researchers are beginning to focus on milder undiagnosed conditions that may also play a role. The list of more subtle factors to be considered includes neurodevelopmental impairment, vestibular dysfunction, attention-deficit/hyperactivity disorder, issues with vision, or other forms of delayed development.
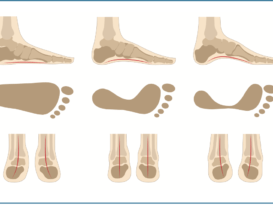
Excluding CP patients, toe walking is estimated to occur at a rate of 7-24 percent in the normal childhood population, appearing in boys more frequently than girls at a ratio approximating 2:1. The literature also shows a positive correlation with family history. Given the array of possible serious contributing factors, ITW is diagnosed by exclusion, i.e., it is essential to first rule out any neurological or orthopedic causes. Examination includes an extensive medical and family history, a neurologic exam, and a thorough biomechanical and gait evaluation. This history includes assessing risk factors from birth, such as pre-natal and postnatal birth weight, prematurity, or any other physiological indications of stress.
Biomechanical Exam
Pediatricians have charts of developmental milestones indicating acceptable age ranges for physical and behavioral signs in infants and children. For example, children normally begin to walk at nine to 15 months of age. Habitual toe walkers follow the regular development of healthy children except that they walk on their toes from the time they
first learn to walk, yet they can come down to flat foot walking on command.
It is not unusual for young children to go through a three- to six-month phase of toe walking and then outgrow it. As part of the overall gait assessment, parents should be asked when the child’s toe walking began and whether the percent of time spent walking on the balls of the feet is generally decreasing or increasing.
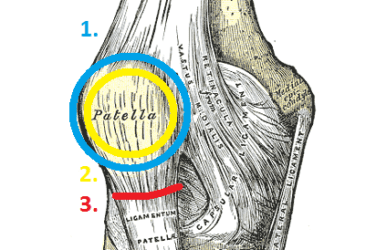
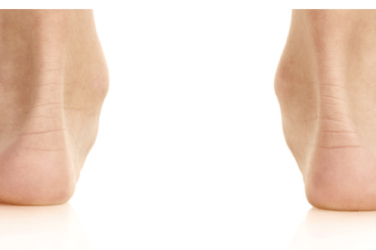
The biomechanical exam should reveal normal foot and leg alignment in all three planes with no excessive torsion or recurvatum of the leg. Development of the lower limb, including muscle strength and tone, should be commensurate with other healthy children. It is important to check range of motion available at the ankle. To rule out equinus, there should be at least 5 degrees of passive dorsiflexion with the subtalar joint held in the neutral position. The Silfverskiold Test can be used to check range of motion and muscle spasticity. Patients with a fixed plantarflexion are unable to get their heels to the ground without severe compensation.
Normal gait can be affected by pain, contractures, and spasticity, and children with sensory issues may prefer to ambulate as toe walkers. Despite the potential serious causes, don’t overlook the obvious. Sometimes a simple plantar wart or an embedded splinter will be the issue. Finally, mimicry—the child copying the gait of another—may be the culprit.
Pedorthic and Orthotic Treatment
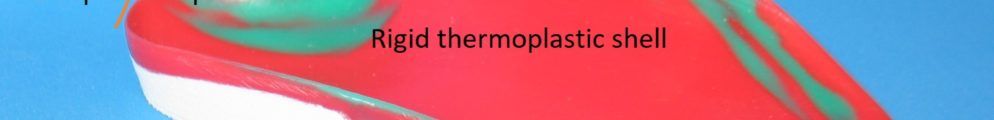
The goal of treatment is to encourage a fluid and stable heel-to-toe gait, correct leg and upper-body positioning, improve balance, and prevent loss of range of motion—particularly at the ankle. Given the long-term consequences of ignoring a plantarflexion contracture, early treatment is encouraged. The best approach will depend on the severity and duration of the condition. For mild cases, pedorthic recommendations such as wearing stiff soled high-tops can be a helpful beginning. Holding the foot down inside the footwear and using a heel-lock lace configuration keeps the foot secure.
Adding a carbon plate under the insole will further prevent dorsiflexion at the metatarsals. Applying a lateral forefoot sole wedge externally discourages adduction. If the child has an element of internal torsion, consider using a gait plate with long lateral extensions inside a sneaker with a flexible sole.
The gait plate can be part of a custom
GAIT EVALUATION
There are some simple clinical tests that may help identify the nature and severity of the condition. As part of the gait analysis, the practitioner should watch the patient walk barefoot and look for the following:
- Can the child take his or her first few steps in a regular heel-to-toe manner, and only resort to toe walking once speed is increased?
- Can he or she stand with both heels on the ground, making full foot contact?
- While toe walking, does he or she display a normal angle and base of gait?
These observations rule out severe equinus or other obvious orthopedic abnormality as causative factors.
In addition, evaluate:
- How high are the child’s heels off the ground while walking?
- Does the child walk in a well-coordinated, efficient, and balanced fashion?
- Can he or she run without tripping?
- Can the child easily walk forward and backward on the balls of his or her feet? In the general population, backward walking is a quick and effective functional gait assessment tool to determine balance, symmetry, and possible neurological deficit.
Difficulty with any of these tests or the appearance of a scissor gait may indicate a neurological component, and the patient should be immediately referred for further investigation. The gait pattern of children who are habitual toe walkers should be similar to those of normal children—except their heels rarely touch the ground. Interestingly, habitual toe walkers are stable and do not fatigue, whereas normal children who elect to toe walk will tire more easily.
Adapted from Caselli, Habitual Toe Walking.1
orthotic or simply a thin rigid flat inlay. These light restrictions act as gentle reminders to the child to alter the gait pattern to heel strike. Finally, lifts under the hindfoot, either inside or outside the footwear, can be used to “bring the ground up,” allowing heel contact to coincide with initial contact. The elevations provide proprioceptive feedback and can be used as a temporary measure. The height should be gradually reduced over time as the issue resolves. Physical therapy and stretching programs are also beneficial and enhance the treatment regimen.
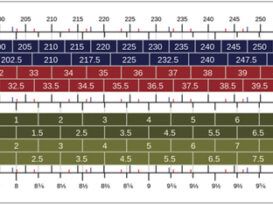
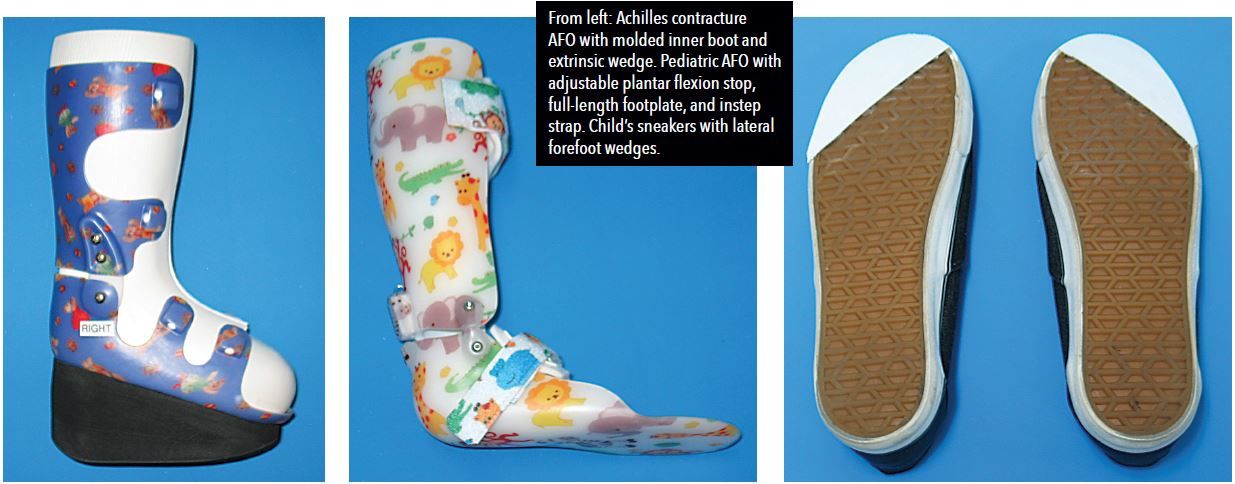
Orthotics, SMOs, and AFOs are frequently prescribed for toe walking cases that are classified as moderate or more severe. In such instances the child may be unable to make heel contact when prompted, or the range of motion may not be available. If the biomechanical exam reveals an underlying forefoot varus, custom foot orthotics or an SMO may be used to address the condition. AFO designs will be patient specific and should involve the physician, physical therapist, and parents. Bracing can be used to limit or block motion at critical joints—the knee, ankle, and metatarsals—as well as controlling pronation and supination of the foot. An AFO with an articulating ankle joint, an adjustable plantarflexion stop, and an instep strap in conjunction with external heel lifts will provide great control that can be adjusted to match the patient’s progress. For significant equinus or Achilles contractures, an AFO with large extrinsic heel wedges can be used as an alternative to serial casting and then easily modified. Night splints have also been used successfully as part of an overall program. In the most severe cases with clear neuromuscular deficits, the final prescription will depend on a host of factors including patient activity level, available range of motion, muscle tone, and overall strength. Other modalities include serial casting, surgery to address the equinus, and Botox injections.
Conclusion
oe walking is not uncommon in the developing child, and most cases will resolve spontaneously. However, toe walking can indicate an ankle equinus or one of many underlying neurodevelopmental disorders. Given the seriousness of these conditions it is essential to rule them out early, and begin simple measures to eliminate any detrimental long term effects. Conservative interventions include pedorthic shoe modifications, physical therapy, custom foot orthotics, and AFOs. Treatment should continue until the child can walk barefoot with full heel-to-toe contact displaying the normal rockers of gait. No long-term studies yet support any one approach, so treatment remains specific to the patient and practitioner.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
References
1. Caselli, M. 2002. Habitual Toe Walking. Podiatry Management.
2. Hand, L. 2017. ITW update: Etiological clues, collaborative care. Lower Extremity Review.