Pedorthists like to maintain that good health starts from the ground up, and it is widely appreciated that foot health is an important key to overall health. This point was underscored again in a recent longitudinal study of 2,110 adults.1 The authors tracked the participants for a mean follow-up of 10.8 years and concluded that within their study group, “taking at least 7,000 steps/day had a 50 percent to 70 percent lower risk of mortality.” Interestingly, there was no association of step intensity with mortality regardless of adjustment for step volume. To put it directly, their results suggest taking at least 7,000 steps per day can extend your life regardless of the speed you walk. Although pedorthics can be viewed as a sub-specialty below the ankle, pedorthists work closely with orthotists and prosthetists to ensure their respective modalities function optimally. O&P facilities and clinics already recognize this natural alliance by employing certified pedorthists and certified prosthetists/orthotists to work side by side providing seamless service to their patients.
Diabetes Crisis
Nowhere is educating the public about foot health and proper shoe fit more important than among people with diabetes who are urged to make foot care one of their top priorities. The statistics on diabetes are staggering, and for decades, with each successive report, the Centers for Disease Control and Prevention shows them rising. In the 2020 National Diabetes Statistics Report, it was estimated there were over 34 million adults in the United States with diabetes. This equates to 13 percent of the US adult population, and the figure rises to over 26.8 percent for adults ages 65 or older. Just behind these sobering numbers it is estimated 88 million people have pre-diabetes. Given that medical costs for people with diabetes are more than twice as high as for those without, the direct economic impact and the burden on the healthcare system is and will continue to be immense. As O&P professionals we recognize the diabetic foot is one of the most serious and costly ramifications of the disease.
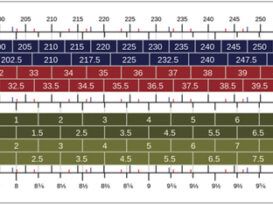
It is very important that people with diabetes take special care with their footwear, especially if their feet are insensate. First and foremost, good shoes must be well fitting with sufficient space in the front—both the length of the shoe and the height of the toe box. It is not unusual for any patient to have slightly different left and right foot measurements, so it is important to always measure both feet and protect the longest toes. The toes should be covered to protect the digits, and the shoe should have a sufficiently stabilizing heel counter. The inside should be seamless, particularly in the forefoot. Extra depth shoes with removable inlays allow modification of the existing insole redistributing the pressure. Depth construction will also accommodate an orthotic if one is prescribed. Patients should be advised to change their shoes daily, not wearing the same pair on consecutive days. This allows shoes to air out, drying any perspiration that may have accumulated, creating a less attractive environment for bacteria and fungus.
Recognizing these benefits, the Medicare Therapeutic Shoe Bill was enacted by Congress in 1993 to provide proper footwear and inserts for people with diabetes who qualify under Medicare Part B. The program has been successful in preventing lower-limb ulcers, amputations, and other complications for many people who suffer from the disease. The approved footwear must be prescribed by a physician and dispensed by a qualified, certified, or licensed clinician, which includes pedorthists and orthotists.

Pedorthic Science and Art
Few people outside the O&P, podiatry, and biomechanics professions have ever heard of pedorthics, and I have learned to explain it as the science and art of fitting shoes and orthotics. The Pedorthic Footcare Association (PFA) (www.pedorthics.org) is the professional body solely dedicated to representing pedorthists, and it can trace its roots back to 1958. At that time the word pedorthic did not exist but evolved from conjoining “ped,” for foot, with orthotist. The PFA defines pedorthics as: The design, manufacture, modification, and fit of shoes and foot orthoses to alleviate problems caused by disease, congenital defect, overuse, or injury. Certified pedorthists (CPeds) are accredited by both the American Board for Certification in Orthotics, Prosthetics & Pedorthics (ABC) and the Board
of Certification/Accreditation (BOC), although only ABC is accepting new applications. Pedorthists work across
the spectrum of the orthotic and shoe industries: fitting customers directly in retail environments, casting, and evaluating patients within O&P facilities, working alongside podiatrists in wound care centers, and working in orthotic and shoe manufacturing and central fab operations. CPeds play an integral role in these inter-dependent networks caring for patients’ feet, their quality of life, and overall health.
On a daily basis pedorthists encounter a wide variety of prescriptions and diagnoses related to the foot, lower leg, and ambulation. Through their extensive clinical education and experience, they dispense soft goods, orthotics, and shoes. The training is quite involved and current education guidelines require attending a course accredited by the National Commission on Orthotic and Prosthetic Education. The syllabus includes sections in anatomy, biomechanics, footwear fitting, lower-extremity orthotic design, manufacturing methods and materials, shoe construction and modification, and patient and practice management. Following the coursework there is a requirement to complete 1,000 hours of residency with certified practitioners. The final stage is passing the ABC written test.
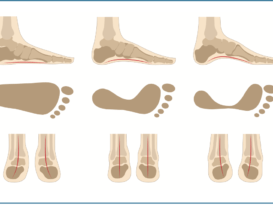
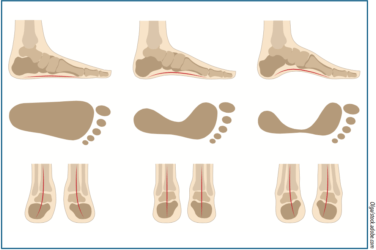
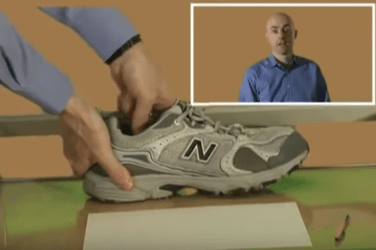
Once in practice, most patient encounters require a pedorthist to take a thorough biomechanical exam of the lower extremity, recognize unique foot anatomy, inspect the feet, and record measurements such as range of motion and plantar pressure. Pedorthists employ worn shoe analysis as another technique. To the trained eye, the wear and breakdown inscribed on old shoes serve as an x-ray of gait, and like a good detective, the pedorthist can see things hidden in plain sight. Foot type, functional hallux limitus, leg-length differences, gait asymmetries can all be inferred from these patterns. A complete evaluation helps determine the appropriate device, materials, and proper positioning of reliefs.
However, pedorthics is also an art. The shoes and orthotics that are delivered must be compatible with the patient’s lifestyle. Beyond the theory, they need to be a practical and functioning solution. Devices that sit in the closet are of no use to anyone. Factors such as a person’s activity level, sense of fashion, and existing shoe gear are of vital importance in developing optimal outcomes. It is through experience and good communication that pedorthists become a valuable link in the patient care chain— recommending, making, and fitting shoes and orthotics that help them walk better and enhance the overall therapy. CPeds are trained in adjusting shoes and there are many tricks and skills to providing foot pain relief using a patient’s existing footwear. Pads, cushions, supports, wedges, and lifts can be deftly added either internally or externally to many regular shoes without altering the cosmetic appearance.
Foot Function
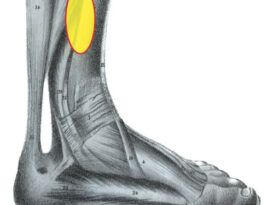
Clinicians that specialize in the lower extremity share the goal of helping their patients walk, and numerous studies link quality of life to foot health. Keeping patients up and ambulating is essential to their health by affecting important diverse factors such as weight management and socialization. Foot dysfunction and, in particular, foot pain have an outsized influence on overall health. Through an understanding of the gait cycle, foot mechanics, and shoe construction, pedorthists can enhance function and mobility in many ways. Orthotics can be fabricated to alleviate pain. Rocker soles can compensate for limited joint motion and restore gait efficiency. Extra depth shoes can be dispensed to protect the feet of people with diabetes and with or at risk of neuropathy. Short trimline AFOs can be used to improve stability and confidence in patients fearful of tripping or falling.
Bunions are one common example of an uncomfortable foot problem. Although it does not present a serious medical problem hallux abducto valgus can make walking painful and shoe fitting very difficult. The condition cannot be reversed without surgery but pedorthists can alleviate some of the symptoms. Selecting shoes with stretchable uppers, generous widths, modifying the last, adjusting the heel fit, and providing medial longitudinal arch support can go a long way toward making the footwear and the patient more comfortable. Hallux limitus is another painful condition that can inhibit physical activity. Conservative treatment includes adding a sole stiffener to reduce dorsiflexion and then compensating for lost range of motion in terminal stance by adding a rocker sole.

Collaboration
One major distinction within O&P is between normal function and rehabilitation medicine. Patients with full function who are active in sports need orthoses to enhance or guide motion, perhaps only limiting end range of motion to avoid pathology. Conversely, when we are trying to address a gross motor deficit, such as with a patient who has had a stroke, we may be forced to sacrifice biomechanical function in favor of stability. Dispensing a solid ankle AFO with a full-length foot plate provides needed support for the weak limb, but it comes at a cost. It limits critical motion at both the ankle and the first metatarso-phalangeal joint, will probably require roomy shoes, and depending on the material thickness, possibly create a leg-length discrepancy. Paradoxically, by focusing on the primary issue, three lesser problems have emerged that certified pedorthists can address. Well-fitting extra depth shoes with rocker soles can accommodate AFOs and restore some of the lost range of motion. With sufficient space, a lift or insole can easily be added to the contra-lateral side to maintain overall balance.
Similarly, prosthetists often struggle with their own competing demands. Consider a patient who uses a left trans-tibial prosthesis and needs a right partial foot prosthesis, but whose feet are different lengths and widths. It may be possible to adjust shoes to get the appropriate fit bilaterally or cast for custom-molded shoes to accommodate for the entirely different foot shapes. Whether receiving a met pad, an extra depth shoe, an AFO, or prosthetic foot, success depends on patient acceptance. Pedorthists, orthotists, and prosthetists working together can develop effective composite solutions.
Conclusion
The fields of pedorthics, orthotics, and prosthetics are natural extensions of each other. Keeping patients on their feet and mobile is fundamental to preventing the progression of many lifestyle-related diseases. Simply by walking, people with diabetes will have improved blood glucose control and weight management. Although comfort may be difficult to define academically, people will not walk if they have pain, balance issues, or fear of injury. Providing proper fitting and stable shoes, foot orthotics or even custom shoes sets the right platform for our patients’ biomechanics and ambulation.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
References
1. Paluch, A., K. Pettee Gabriel, J. Fulton, et. al. 2021. Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study, 4(9):e2124516. JAMA Network Open (doi 10.1001/jamanetworkopen.2021.24516).