On a daily basis, orthotists, pedorthists, and prosthetists deliver an array of devices and care that markedly improve their patients’ quality of life, and many in the profession take deserved satisfaction in witnessing these successful outcomes. For some it is the ultimate reward for the hard work and dedication it took to develop their craft and expertise. Most practitioners can readily recall life-changing encounters fitting an orthotic and seeing a patient’s mobility restored, their pain eased, or independence regained. Those special moments are the magic of what we do.
Although we intuitively understand the value of this care, it remains important to study and document the benefits to be recognized by the wider healthcare and reimbursement community.
Evidence-based medicine (EBM) is a term that has been in use since the 1990s. According to Johns Hopkins University, it is the integration of the best research evidence along with clinical expertise and the inclusion of patient values, often represented as a Venn diagram of three intersecting circles. The EBM model proposes that the best care comes when practitioners, having honed their clinical judgement, are also aware of the current scientific evidence. This in turn guides them to treat the specifics of each case presented while respecting the uniqueness of the patient and his or her preferences.
This article is the third in an occasional series that highlights some of the research supporting the use of foot orthotics. Like the first two installments (July 2011 and September 2016), it underscores the scientific basis for using foot orthotics for a wide range of maladies. The summary of each paper was adapted directly from its abstract.
Low Back Pain
Chronic low back pain (LBP) is one of the most common reasons people will see a doctor or miss days at work. According to the World Health Organization, the lifetime prevalence of LBP in industrialized countries is estimated to be 60-70 percent, resulting in an immense economic cost.
It is widely believed that nonspecific LBP (i.e., not associated with a trauma or obvious musculoskeletal disease) is a result of a combination of factors. If the nature of the ailment is recurring, there is good evidence to consider the cause may be related to posture, a leg length discrepancy, a functional asymmetry, or gait blockage in the sagittal plane. Any of these anomalies that restrict ideal movement can focus stress or overwork the mechanisms of the lower back. Orthotic treatment of LBP seeks to restore full function, range of motion, and symmetry so the body moves naturally and pain free.
1. Chronic low-back pain and its response to custom-made foot orthoses. 1999. H. J. Dananberg, M. Guiliano. Journal of the American Podiatric Medical Association 89(3):109-17.
A new approach to treating chronic low-back pain with custom-made foot orthoses was investigated. The Quebec Back Pain Disability Scale was used to objectively assess the functional disability of 32 subjects at different times. Subjects in this prospective study experienced more than twice the improvement in alleviation of pain, and for twice as long, compared with subjects in a study using traditional back-pain treatment.
2. The effect of insoles on the incidence and severity of low back pain among workers whose job involves long-distance walking. 2005. S. Shabat, T. Gefen, M. Nyska, Y. Folman, R. Gepstein. European Spine Journal 14(6):546-50.
In this double-blind prospective study, the effectiveness of insoles constructed in a computerized method were compared to placebo insoles. There were 58 employees whose work entailed extensive walking and who suffered from LBP. This study demonstrated that the LBP decreased significantly after using real insoles compared to placebos.
3. LBP and lower limb discrepancy: 3D evaluation of postural rebalancing via underfoot wedge correction. 2012. Moreno D’Amico, Piero Roncoletta, Francesca Di Felice, Daniele Porto, Rosagrazia Bellomo, Raoul Saggini. Studies in Health Technology and Informatics 176:108-12.
Leg Length Discrepancy (LLD) is very often associated with LBP, but the use of heel lifts to re-balance pelvis and trunk posture remains controversial. In a review of five years of clinical activity it was observed that more than 70 percent of 300 LBP patients presented with a LLD. More than 80 percent measured the presence of asymmetric foot loading in stance. A longer lasting recovery effect was observed when LLD correction was adopted. From a sample of 94 LBP patients, 83 (88 percent) were found to improve posture when LLD was corrected. Data comparison showed significant postural improvements could be obtained in whole or in part both in rebalancing and in spine deformities reduction with the application of suitable heel lift.
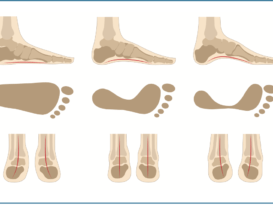
4. The short-term effect of custom-made foot orthoses in subjects with excessive foot pronation and lower back pain: a randomized, double-blinded, clinical trial. 2013. Aurora Castro-Méndez, Pedro V. Munuera, Manuel Albornoz-Cabello. Prosthetics and Orthotics International 37(5):384-90.
A sample of 51 participants with excessive subtalar pronation and chronic LBP were selected. The effect of custom-made foot orthoses on LBP was studied over a four-week period. The study design was a randomized, double-blinded, clinical trial with two groups. In the sample studied, the use of custom-made foot orthoses to control foot pronation had a short-term effect in reduction of perceived LBP.
5. Shoe Orthotics for the Treatment of Chronic Low Back Pain: A Randomized Controlled Trial. 2017. Jerrilyn A. Cambron, Jennifer M. Dexheimer, Manuel Duarte, Sally Freels. Archives of Physical Medicine and Rehabilitation 98(9):1752-1762.
The objective of this study was to investigate the efficacy of shoe orthotics with and without chiropractic treatment for chronic LBP compared with no treatment in a randomized controlled trial. Adult subjects (N=225) with symptomatic LBP of ≥3 months were recruited from a volunteer sample. Subjects were randomized into one of three treatment groups (shoe orthotic, plus, and waitlist groups). The shoe orthotic group received custom-made shoe orthotics. The plus group received custom-made orthotics plus chiropractic manipulation, hot or cold packs, and manual soft tissue massage. The waitlist group received no care. Six weeks of prescription shoe orthotics significantly improved back pain and dysfunction compared with no treatment. The addition of chiropractic care led to higher improvements in function.
Knee Pain
Although exact numbers are difficult to determine, mechanical knee pain accounts for a significant portion of exercise-and running-related injuries. In addition, older patients frequently experience knee pain as a result of osteoarthritis. Knee pain is a complex subject, and the leading researchers advance more than one theory of etiology. It is probable that there may be subgroups within patient cohorts who respond differently to treatments. For example, women are far more likely to experience patellofemoral pain than men, and teenage girls are at more than twice the risk compared to boys. The underlying cause of knee pain is an area rich in opportunity for investigation and much work needs to be done to develop a comprehensive theory and patient-specific treatment protocols. However, there is good evidence supporting the use of orthotics, both custom and prefabricated, for these patients.
Conducting high-quality research directly furthers the science of the service our profession provides. It does not have to be complicated. Well-designed studies with simple objectives can have profound effects on our understanding and demonstrate our unique role in enhancing human movement. Engaging the principles of EBM is a dedication to life-long learning, and it can involve a commitment to the continuing education
of other professionals and our patient communities. The papers outlined here are a starting point for the body of work that already exists.
Watch for Part IV of the series coming in the June issue.
For those interested, PubMed, pubmed.ncbi.nlm.nih.gov, is a free search engine and database of references and abstracts on life sciences and biomedical topics.
1. Effects of prefabricated foot orthoses on pain and function in individuals with patellofemoral pain syndrome: a cohort study. 2011. Barton, C. J., Menz, H. B., Crossley, K. M. Physical Therapy in Sport 12(2):70-5.
This study evaluated the effects of unmodified prefabricated foot orthoses over a 12-week period on functional performance; and subjective pain and function in individuals with patellofemoral pain syndrome (PFPS). There were 60 individuals with PFPS (18-35 years). At 12 weeks, significant improvements in a) single-leg squat pain and ease, b) the number of pain-free step downs and c) single-leg rises from sitting were found. Functional performance improvements following unmodified prefabricated foot orthoses were greater at 12 weeks than those achieved immediately. Enhanced functional performance over time may have significant implications for osteoarthritis prevention in some individuals with PFPS. Improvements in subjective pain and function appear to plateau over time.
2. Benefits of custom-made foot orthoses in treating patellofemoral pain. 2011. Munuera, P. V., Mazoteras-Pardo, R. Prosthetics and Orthotics International 35(4):342-9.
Twenty-one subjects with patellofemoral pain (PFP) were given custom-made foot orthoses (2-mm thick polypro and 4-mm thick polyethylene foam liner of 45 shore A hardness). PFP was evaluated with a visual analogue scale before applying the treatment, and at two weeks and four weeks follow-up. At the two-week check-up, a forefoot varus posting was added to the orthoses. Improvements in PFP was significant in all comparisons: initial pain with pain at the two-week check-up, initial pain with pain at four weeks, and pain at two weeks with pain at four weeks. The effect size was large in all comparisons. For the participants in this study, the custom-made foot orthoses were found to be an effective conservative treatment to reduce the symptoms of patellofemoral pain.
3. Custom-Made Foot Orthoses Decrease Medial Foot Loading During Drop Jump in Individuals With Patellofemoral Pain. 2016. Rathleff, M.S., Richter, C., Brushøj, C., Bencke, J., Bandholm, T., Holmich, P., Thor- borg, K. Clinical Journal of Sport Medicine 26(4):335-7.
The authors investigated the effect of custom-made foot orthoses on medial-to-lateral plantar forces during drop jumps and single-leg squats and explored the self-reported change in symptoms after 12 weeks of wearing the orthoses in individuals with patellofemoral pain (PFP). They evaluated 23 adults with PFP. This preliminary study showed that foot orthoses were associated with a decrease in medially directed foot loading among individuals with PFP. Individuals who have an immediate decrease in the medial-to-lateral peak force after fitting the orthoses were more likely to report improvements after 12 weeks of use.
4. The effect of orthotic devices on knee adduction moment, pain and function in medial compartment knee osteoarthritis: a literature review. 2017. Roshanak Baghaei Roodsari, Ali Esteki, Gholamreza Aminian, Ismaeil Ebrahimi, Mohammad Ebramim Mousavi, Basir Majdoleslami, Fatemeh Bahramian. Disability and Rehabilitation: Assistive Technology 12(5):441-449.
The aim of this review was to evaluate the effects of foot orthoses and knee braces on knee adduction moment, pain and function in individuals with knee osteoarthritis (OA). Thirty-one related articles were selected for final evaluation. The results of the analysis of these studies demonstrated that orthotic devices reduce knee adduction moment and also improve pain and function in individuals with knee OA. In conclusion: Foot orthoses may be more effective in improving pain and function in subjects with knee OA. The combined use of a knee brace and foot orthoses provided more improvement in knee adduction moment, reduced pain, and increased function.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.