Previously, I provided an overview of early foot-orthotics theory, as well as a brief history of arch supports. Seminal work by Merton Root, DPM, on the relationship of the subtalar joint (STJ) to the midtarsal joint, neutral-position slipper casting, and foot orthotic modifications has been foundational to the modern custom foot-orthotic industry. Although not a complete description of the foot in motion, nor of the causes of biomechanical foot pathology, Roots work developed a framework upon which others could build. This article outlines two concepts that further enhance the knowledge of foot-orthotic biomechanics.
Joint Motion
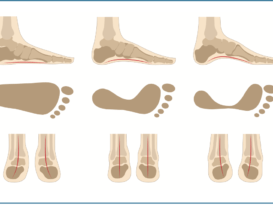
Current research shows conclusively that the motion of the foot and ankle is remarkably complex. This is hardly surprising, considering that each foot consists of more than 100 ligaments and 26 bones, plus numerous muscles and bony articulations. Early work was confined to considering restricted joint motion because the complexity of the foot was not fully understood. For example, the ankle is obviously involved in sagittal plane motion; this is what enables the body to move over the weight bearing foot. However, it is now clear that the ankle also has motion in the frontal and transverse planes. This is important in understanding that the movement of the heel relative to the lower leg is not solely due to the STJ.
Given the triplanar motion of the ankle, the ligament support structures play a vital role in guiding the motion at the ankle and rearfoot, and that motion is not restricted solely to the articular surfaces of the rearfoot. Unlike foot orthotics, traditional AFOs address this fact by potentially limiting range of motion in all three planes. Recognizing that the ankle is not simply a “hinged plate” helps further our understanding of its function and opens possibilities for optimal orthotic designs. The development of the Richie Brace is an example of this.
Study of the STJ also shows that there is motion between the calcaneus and talus in all three planes. This range of motion (ROM) depends on the current position of the joint; i.e., there is a range of ROM based on the actual position. The motion of the talus and calcaneus is closely guided by their facets, and cadaver studies show that STJ motion characteristics vary among subjects. This variance is important because STJ motion directly affects ankle and midtarsal joint motion. The midtarsal joint, which is the combination of the talonavicular and calcaneocuboid joints, is a functional rather than anatomical joint. It is seen as a single functional unit and displays considerable ROM in all directions.
Traditionally, articulations of the midfoot were not considered independently, but the indications are that all parts of the foot (navicular, cuboid, cuneiforms, metatarsals, and digits) move in relation to one another and are important to biomechanical foot function. Beyond joints, there are other factors influencing foot function that are not fully understood, such as the role of soft tissue and the intrinsic muscles.
Although somewhat technical, this review is meant to remind readers to keep their understanding of foot biomechanics open, beyond the standard Root-STJ model. Lower-limb biomechanics and joint motion are not limited to one or two conceptual models. (Editor’s note: For more information, as well as a bibliography on this subject, read “Redefining Biomechanics of the Foot and Ankle,” Podiatry Today , October 2005.)
Tissue-Stress Approach to Biomechanics
Over the past two decades, a new concept in biomechanics has emerged that looks at the forces acting on the weight bearing foot, rather than at joint position or motion. Referred to as the “tissue-stress” approach to biomechanics, this concept uses the principles of physics to explain why a foot moves in a particular way and why that may cause pain. Tissue-stress examines forces on anatomical structures. By examining the weight bearing foot, we can see what the ground reaction force (GRF) will attempt to do. Our goal then becomes to design orthotics that reduce or relocate the forces, eliminating the stress.
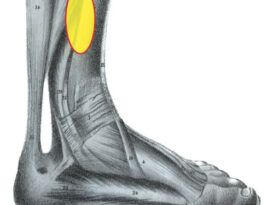
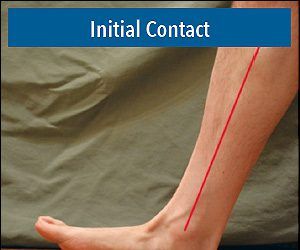
As a quick reminder, a force (F) that causes an object to rotate is said to contribute a moment (M) to the object. The magnitude of a moment can be found by multiplying the magnitude of the force (F) by the appropriate moment arm, or distance (d). That is: M = F x d. This creates a torque around the pivot point (see figure 1).
 |
| Figure 1 Tissue Stress Foot Biomechanics |
Thus, we need only to determine the location of the center of pressure (CoP) within a foot and the orientation of the subtalar joint axis. The acting GRF can be averaged to a single point. Although we may not be able to pinpoint their locations exactly, we can see that if the CoP is located laterally to the STJ axis, the GRF will try to pronate the foot. Likewise, if the CoP is located medially to the STJ axis, the GRF will try to supinate the foot. When the CoP is directly beneath the STJ axis, there will be no moment, or torque, from the GRF.
GRF is not the only source of moment acting on the STJ axis. Muscles create moments as well. For example, a medially deviated STJ axis tends to have a pronatory effect. In some cases, the posterior tibial (PT) muscle, which is a prime supinator of the STJ, deploys to counteract this moment. Thus, the pronation moment from the GRF is resisted by the supination moment of the PT muscle. In the long run, if the pronation moment is great enough, this could lead to posterior tibial tendon dysfunction (PTTD). Other factors that can provide resistance moments to the GRF are the action of the plantar fascia and bone-on-bone end of ROM.
Understanding these principles shows us how to reduce moments and relieve symptoms. The net moment determines the direction and degree of rotation. By identifying the anatomical structure that hurts, you can design an orthotic that reduces or shifts the stress from that location. Extrinsic wedges or posts, pads, cast skives, and shoe modifications can all be used to shift the CoP in relation to the STJ axis. Footwear also plays a critical role in transmitting GRFs and in determining the effectiveness of foot orthotics.
Adding a medial rearfoot wedge to an orthotic, for example, moves the center of pressure more medially. This increases the supination moment about the STJ axis, helping to support the foot. The tissue-stress theory also explains why a rearfoot medial wedge is more beneficial than a forefoot medial wedge: it is located farther away from the STJ axis, which increases the moment arm.
Similarly, a forefoot lateral wedge will increase the supination moment, potentially offsetting the effect of a laterally deviated STJ axis. This provides the greatest reaction because it is located farthest from the STJ axis, maximizing the moment arm. It also has the added benefit of working later in the gait cycle.
This is only a brief summary of the work done by, among others, Eric Fuller, DPM, and Kevin Kirby, DPM, MS, while at the California College of Podiatric Medicine. A more comprehensive description of this theory is available in Fuller’s article, which appears in the January 2003 issue of Podiatry Management.
Future research will doubtless build on these emerging concepts and validate what many clinicians intuitively know. In the meantime, close observation and experience will allow practitioners to design appropriate devices to help their patients, regardless of any particular theory.