Heel pain is one of the most common reasons people seek medical care for the foot and ankle, and in its advanced stages it can be debilitating. It is also very treatable, and numerous studies demonstrate the success of a variety of conservative measures including foot orthotics, physical therapy, and taping. As there are many possible causes of heel pain, a careful diagnosis is essential to appreciate each of the contributing factors and its true etiology.
Plantar Fasciitis
Plantar fasciitis is reported as the most frequent cause of heel pain, and one of its more common telltale signs is patients reporting that it is worst in the morning when they first step out of bed. They may also say the pain is greater when they stand up after sitting down for an extended time. This post-static dyskinesia occurs when the unloaded plantar fascia shortens then, upon standing, it is suddenly stretched. As weight bearing activities continue, the pain usually lessens, and this can be a key observation in isolating the cause.
Classic plantar fasciitis is usually seen as a deep tender pain that sometimes radiates into the arch. There is often pain along the fascia and in particular at the medial calcaneal insertion. The term plantar fasciitis was originally developed because it was assumed that most heel pain was an inflammation response either to overuse or trauma. The current thinking is that plantar fasciitis is a chronic degenerative-reparative process that is brought on by stress overloading, although the exact causes can be varied and multifactorial. As a result, the newer terms plantar fasciopathy or fasciosis are considered more accurate.
Heel spur is another popular term used to describe the condition, however not all patients with plantar fasciitis develop calcaneal spurs. Several studies have indicated that 30-60 percent of patients with heel pain do indeed have a spur. But a significant minority (15-20 percent) of control groups with a spur do not have heel pain. Clearly the presence of a spur is not the definitive factor. Further investigation reveals that plantar fascia thickening (> 4mm) is twice as likely to be associated with heel pain compared to a calcaneal spur, and in approximately one-third of cases both are found together. Researchers now believe that the spurring may be a response rather than a cause of heel pain, and plantar fascia thickening precedes it.
Nerve Entrapment
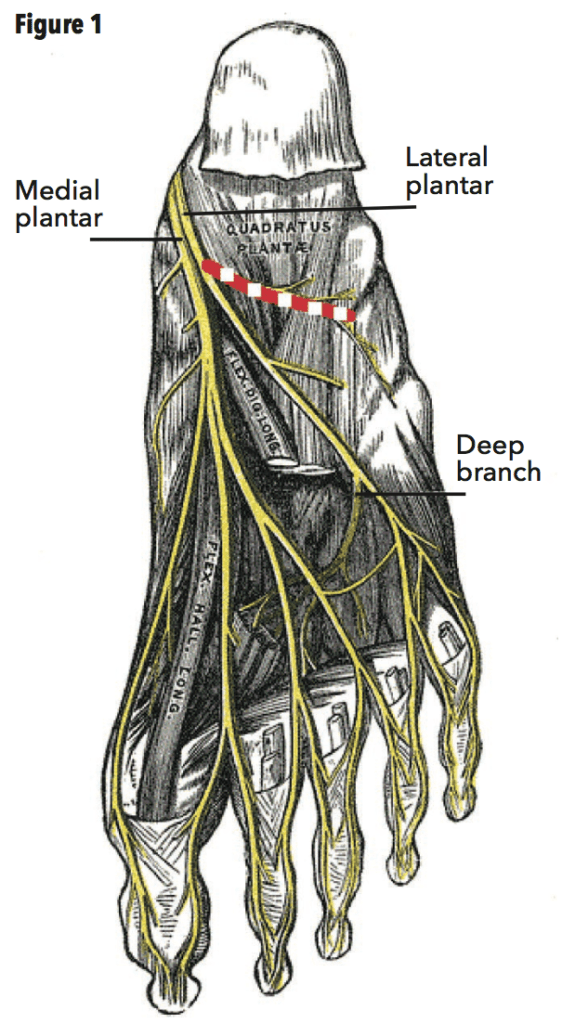
Although the majority of heel pain cases are related to issues with the plantar fascia, it is important to rule out other ailments and conditions. The posterior tibial nerve has several divisions at the level of the calcaneus. The medial calcaneal branches are sensory and do not innervate the plantar fascia. Patients with complaints of medial posterior heel pain that is not worse with the first few steps and pain that does not resolve after walking may have neuritis of the medial calcaneal nerve. Just distal to this, the second branch, the inferior calcaneal nerve (formerly referred to as the first branch of the lateral plantar nerve), takes a precarious course underneath the heel as it traverses from medial to lateral (Figure 1). Entrapment of the inferior calcaneal nerve is commonly known as Baxter’s neuropathy. The nerve passes through a corridor with the plantar fascia and muscle below and the calcaneus, muscle attachments, and long plantar ligament above. Degeneration of any of these structures can easily compress this nerve, supporting the notion that heel pain can be multifactorial. For example, thickening of the plantar fascia in response to mechanical stress may lead to a narrowing of the tunnel resulting in nerve compression.
Other Diagnoses
Stress fracture: The presence of a calcaneal fracture can be initially identified by the heel-squeeze test. Hold the medial and lateral heel in your cupped hands and gently apply pressure to the walls of the calcaneus. The patient will quickly report pain from the compression. Patients with stress fractures will not report a lessening of symptoms as they continue walking during the day, and they may be able to recall an incident of trauma or overuse that initiated the pain.
Tarsal tunnel syndrome (TTS): TTS results from compression of the posterior tibial nerve, and frequently the pain increases with activity and worsens as the day progresses. As the symptoms include pain, burning, and numbness, mimicking neuropathy, it can sometimes be overlooked in people with diabetes. However, unlike most peripheral neuropathy, TTS often presents unilaterally. A quick test for TTS is a positive Tinel’s Sign, which produces a shooting tingling sensation in the distal limb when the skin is tapped with a finger along the course of the posterior tibial nerve. The nerve compression may be a result of previous trauma, a degeneration of the support structures of the foot related to adult acquired flatfoot, overuse, or a growth or cyst within the tarsal tunnel.
Fat pad atrophy: Older patients and heavy patients with thin, reduced plantar fat pads may relate heel pain that worsens after prolonged walking or standing. They might have diffuse pain around the heel bilaterally and complain of pain at night or when at rest. The symptoms can often be eased with a reduction in activity, cushioned inserts, deep heel cups, and proper foot gear.
Various forms of arthritis and degenerative joint disease should also be considered in the differential diagnosis, and more extensive examination with radiographs and EMG nerve conduction tests may be required. For example, radiculopathy, a pinched spinal nerve, can sometimes contribute to heel pain. Finally, an acute tear to the plantar aponeurosis can result in pain. This is not unusual in athletes or after a traumatic event and can be confirmed with an MRI.
Risk Factors
Some segments of the population are more prone to developing plantar fasciitis. Among the more likely groups are those who stand on hard, unforgiving, flat surfaces, for example, traditional factory workers or waitstaff. Athletes, and in particular distance runners, are also at risk, especially if they have recently increased workout intensity or significantly changed training patterns. Weight gain, which adds to the incremental loading on the foot, can be another factor. Women suffer from plantar fasciitis at greater rates than men, and it is more prevalent in middle age.
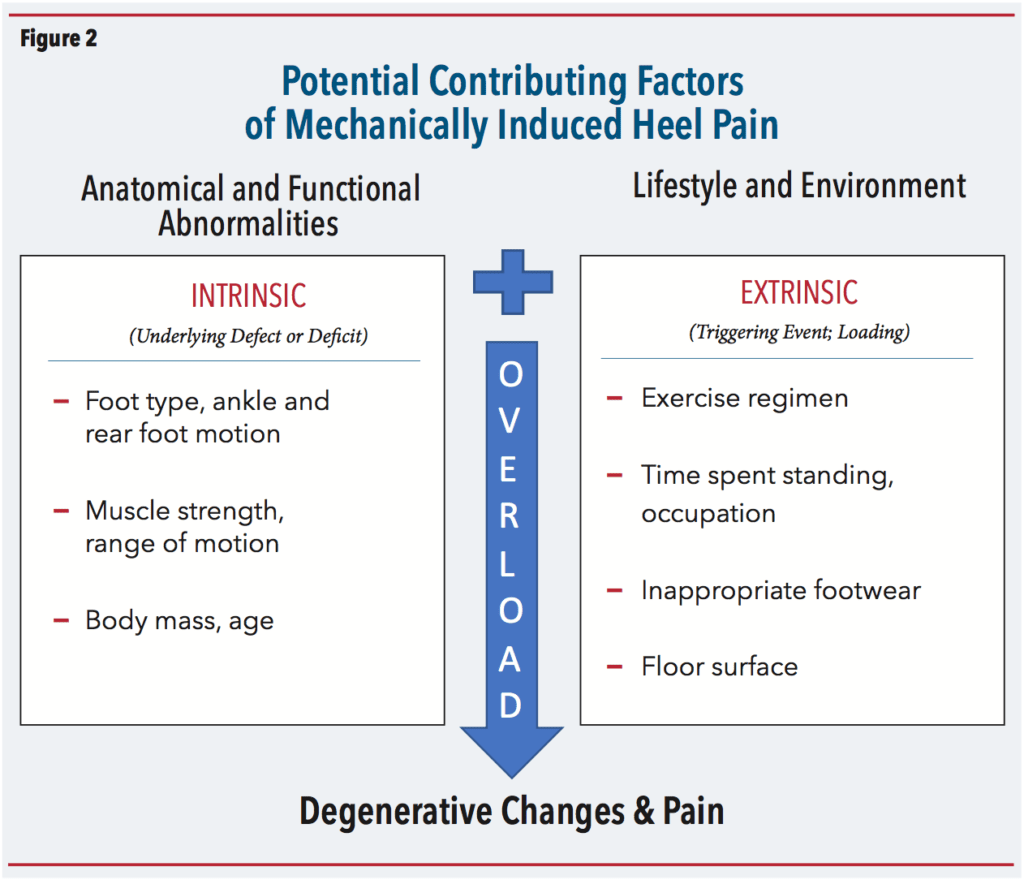
More recent research has begun to identify both intrinsic and extrinsic factors that contribute to the phenomenon of heel pain (1). Intrinsic predisposing factors include anatomical or functional constraints such as range of motion deficits, muscle imbalance, mal-alignment of the foot and lower leg, and body mass. Extrinsic considerations refer to lifestyle and environment, the loading factors that increase the risk. Occupation, exercise level, footwear, and any recent changes in these all have their effects (Figure 2). It is believed that combinations of these factors contribute to the development of heel pain. Interestingly, heel pain often presents unilaterally, even though there is no significant difference in loading from left to right. This underscores the need for a thorough biomechanical evaluation to identify the specific root causes.
Mechanics
Foot mechanics are of primary concern among the causative factors in the development of plantar fasciitis. Strain in the plantar aponeurosis occurs for many reasons, and plantar fasciitis is associated with several different foot types. After initial heel contact the normal foot pronates. This unlocks the subtalar joint (STJ), absorbs shock, and allows internal tibial rotation. Later in the cycle, the foot resupinates in preparation for propulsion and swing. Patients with obvious eversion and calcaneal valgus in the terminal phase of gait are failing to resupinate the STJ and stabilize the midfoot in a timely manner. This puts excessive strain on the plantar fascia. Conversely, high-arched foot types are unable to adequately evert. They maintain a rigid or partially compensated foot structure that can put undue strain on the fascia throughout the cycle. In addition, a leg length discrepancy or ankle equinus can exacerbate fascia band tension.
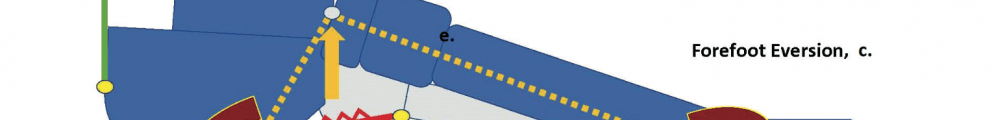
It may seem somewhat contradictory that a high-arched, rigid foot and its opposite, a foot prone to eversion, would both develop symptoms of plantar fasciitis. Kogler et al. provided an explanation for this in a 1999 study (2). Cadaver feet were positioned on a loading frame and a strain transducer was imbedded into the central band of the plantar fascia. Placing medial wedges under the forefoot significantly increased strain in the plantar aponeurosis, but lateral wedges decreased it. This was a controversial finding and contrary to accepted belief at the time. It suggests that orthotics with forefoot lateral posting reduce strain on the plantar fascia (3). Although not intuitive, it means pronation of the forefoot relative to an inverted rearfoot actually lessens tension in the aponeurosis. It seems the primary biomechanical fault causing strain on the plantar fascia has more to do with the forefoot-to-rearfoot relationship than a specific foot type.

Orthotics and Footwear
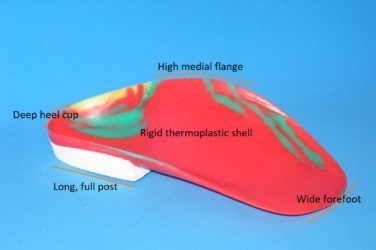
The good news is heel pain that is mechanical in origin potentially has a mechanical solution. Many research papers show the benefits of orthotic therapy in treating plantar fasciitis (4). If the etiology of the dysfunction can be determined from examination, then a properly designed foot orthotic can alleviate the symptoms. The skill is in identifying and isolating the major contributing factor. A well-fitting and comfortable semi-rigid orthotic, suitable to the patient’s lifestyle, can be essential to healing the condition. In principle, an orthotic that inverts the rearfoot and adducts the forefoot reduces stress in the plantar fascia, and the literature supports the use of both prefab and custom devices. For example, for patients with an everted foot, consider some combination of good medial arch support, extrinsic rearfoot posting, and an intrinsic medial heel skive. The relative position of the forefoot can be accommodated with distal extensions such as a sulcus post or a reverse Morton’s. Deep heel cups (> 18mm) are used to limit calcaneal fat pad displacement and provide more rearfoot control. Equinus, often a contributing component, can be addressed with heel lifts that should be dispensed bilaterally to avoid creating a leg length discrepancy. In cases where the medial aponeurosis is inflamed and tender, a plantar fascia groove may provide some relief.
Some patients respond well to the addition of heel cushions or heel spur U-shaped cutouts. The padding may relieve point pressure and also helps by elevating the heel. It is also important to consider the shoes that will be worn. Supportive shoes with a removable inlay, firm counters, and heel-toe drop or offset of 10-12mm provide a good foundation for an orthotic device. In the case of runners, if there are signs of obvious wear or midsole compression, you should advise getting new sneakers. It is recommended the midsole not be too soft, but the shoe itself should flex easily at the metatarsal heads. Stiff-soled shoes prevent dorsiflexion of the hallux and digits, inhibiting the synergistic action of the windlass mechanism.
Other Therapies
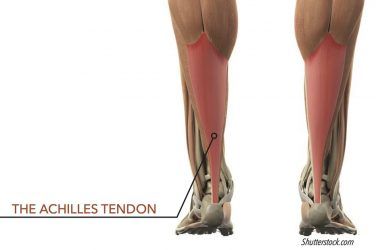
Beyond orthotics there are a variety of other approaches to address the mechanical and soft tissue aspects of heel pain. Initially, rest and icing are recommended. Tight muscle groups directly limit joint range of motion, putting excessive strain on adjacent structures. Conceptually the leg can be considered as a single unit with simple hinge components at the foot, ankle, knee, and hip. During ambulation the extent of motion will be determined by the tightest or most restricted joints. In such a case, the chain is not as strong as its weakest link, but rather it is only as free as its tightest link. For example, a relatively tight or short Achilles tendon causes a functional equinus, which in turn may result in calcaneal eversion leading to heel pain. A heel lift may be all that is necessary to resolve this.
Physical therapy targeted at specific muscle groups such as the gluteals, hamstrings, or triceps surae has proven successful to help ensure adequate joint mobility. Home stretching exercises are often prescribed, and patients play a critical role in their own recovery based on how faithfully they follow the regimen. Stretching needs to be done correctly and consistently, several times a day, if it is to be effective. A gradual approach with stretches that are slow, long, and static is preferred as the patient builds recovery. The objective is not to elongate the plantar fascia but to stretch the soft tissues that are restricting motion in the lower limb.
There is good evidence that low Dye strapping helps reduce heel pain. Correct use of taping can be effective, and it is thought that it has both a mechanical and proprioceptive component. Physicians can also prescribe night splints, extracorporeal shock wave therapy, laser therapy, and injections. More advanced stubborn cases may require cortisone injections, anti-inflammatory drugs, and ultimately surgery as a last resort. Studies show up to 90 percent of instances of heel pain are resolved by conservative measures when patients adhere to treatment protocols over several months.

Conclusion
Researchers are aware that no single factor or event predicts the onset of heel pain and likewise no standalone treatment guarantees a cure. Put more simply, no one model is predictive of pathology, and many now believe a combination of intrinsic and extrinsic factors are likely implicated. Each instance of heel pain needs to be treated on an individual basis. Foot mechanics, degeneration of the aponeurosis, thickening of the fascia, and nerve entrapment are all candidates in the cascade of events leading to heel pain. Combinations of treatment including orthotics, rest, physical therapy, and medicine have been shown to address the condition and reverse the cycle of pain. Effective, long-lasting treatment targets the underlying causes and not just the symptom.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
References
1. Wearing, S. 2019. Rethinking the treatment algorithm for plantar fasciitis. Podiatry Today 32(11).
2. Kogler, G. F., F. B. Veer, S. E. Solomonidis, and J. P. Paul. 1999. The influence of medial and lateral placement of orthotic wedges on loading of the plantar aponeurosis. Journal of Bone and Joint Surgery American 81(10):1403-13.
3. Kennedy, S. 2021. Arch mechanics and the plantar fascia. The O&P EDGE 20(9):46-50.
4. Kennedy, S. 2011. The effectiveness of foot orthotics: Part 1. The O&P EDGE 10(7):46-50; and 2016. The effectiveness of foot orthotics: Part 2. The O&P EDGE 15(9):70-76.