Orthotics are used to prevent or correct deformities, support and align the body, or improve its function. Functional foot orthotics are in-shoe devices that control, guide, or limit the motion of joints and muscles in the foot and ankle, and proximally along the closed chain from the leg to lower back. They are prescribed to alter the magnitude, timing, and duration of forces acting on the foot, and as a result reduce the severity of mechanical pathology. They are indicated for a range of issues and are proven to be very successful in minimizing pain and tissue destruction by returning the foot to a more normal or ideal function.

The primary considerations in the design of any foot orthotic are the physician’s prescription and the diagnosis. In reality, the process is complicated by findings from a full biomechanical examination plus other demands such as the patient’s footwear, lifestyle, and activity level. The top section of most orthotic lab prescription forms requests patient information that directly influences and informs the decision-making. One of the most important details is the patient’s weight, which, along with shoe type, allows the technician to make several critical decisions.
Shell Specifications
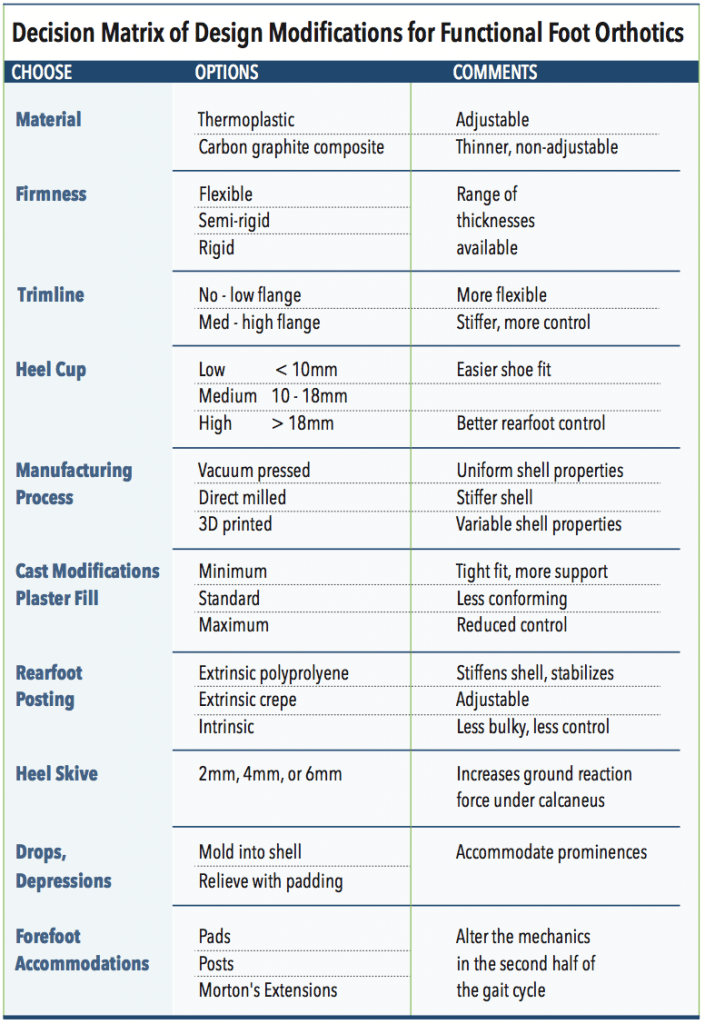
In the absence of clear directions, a typical functional foot orthotic would be formed from thermoplastic, made semi-rigid, and ground to standard width. Most labs rely on their own standards, which work reasonably well most of the time. Shell specifications determine the amount of control the shell provides: flexible, semi-rigid, or rigid. This is determined by several factors including the choice of material, the thickness of that material, the width and contour of the shell, the method of manufacture, and the patient’s foot type.
Materials
The two most common functional orthotic materials are thermoplastics and carbon graphite composites. Although there is a wide variety of both, graphites tend to be stiffer than plastics for a given thickness. This makes them preferable in cases where space inside the shoe is of concern. However, carbon graphites are thermosets and once formed, unlike thermoplastics, are very difficult to adjust.
Firmness
The patient’s weight and activity level determine the load on the plate and subsequently the amount of deformation. The stiffness of any material is in proportion to its thickness: The thinner the material the more flexible it will be. Stiffness is also directly influenced by the final trim lines of the plate. Much like a plank, a long flat orthotic shell will bend more easily than one that is shorter and curved, so the actual size of the foot also plays a role. Engineers refer to this resistance to bending as the area moment of inertia (I). Regardless of the control they exert on the foot, the addition of a flange or heel cup increases the value of I and reinforces the strength of the shell.
Trimlines
Orthotics with high medial flanges, originally called Shaffer plates, are stiff. They are more readily tolerated by patients with non-rigid flatfeet. Alternately, orthotics with lateral walls can work well for higher arched feet and may limit inversion ankle sprains. Maintaining a wide or broad distal platform also provides more control under the medial column just as heel rise begins. Many of these stabilizing features are incorporated into pediatric orthotics as both children’s shoes and their feet are more forgiving.
Heel Cup
Although there is no industry standard for heel cup height, 10mm
or less is generally considered low or shallow. Lower wall heights offer less control, but the device fits more easily into dress shoes. Deeper heel cups, 18mm and higher, have greater contact surface area to provide more rearfoot control and are helpful when there is hindfoot eversion.
Manufacturing Method
The manufacturing process itself also affects the final shell properties. An orthotic that is direct milled from a block of polypropylene will be firmer than a plate of the same thickness that has been oven heated and vacuum pressed. 3D printing introduces new variables into the design process as variations in material performance are possible and opens new worlds of creativity for orthotic production. 3D printing can vary shell thickness, and therefore flexibility, under targeted regions of the foot. This allows for firm support where the load is greater and a thinner less bulky shell elsewhere.
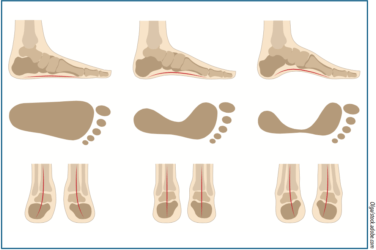
Finally, the patient’s foot type is a key consideration. Rigid feet or those with significant equinus will not usually tolerate hard orthotics as they often cause pain and are rejected. Some level of forgiveness from the shell may need to be provided—even if at the expense of less control. On the other hand, non-rigid, correctable feet can adapt to firm support as is the case with hypermobile pediatric flatfeet, which often respond well to rigid, high-walled UCBLs.
Plaster Fill
The development of modern foot orthotic theory began in the 1950s with the work of Merton Root, DPM, and colleagues. One of the cornerstones of their work was the subtalar joint (STJ) neutral plaster slipper cast. The calcaneus is brought to the STJ neutral position and the fourth and fifth metatarsal heads are loaded, putting the midtarsal joint in maximum pronation. This captures the frontal plane angulation of the forefoot in relation to a neutral rearfoot and provides the reference for fabricating a functional orthotic. Following Root theory, labs build an anterior platform across the metatarsal heads while maintaining a vertical calcaneus. Thus, a pronating foot with forefoot varus, where the first metatarsal head is elevated off the ground, requires plaster build up on the medial side blending to zero on the lateral side. An orthotic formed over a plaster positive that has been balanced in this manner will raise the base of the first metatarsal.
Labs apply some amount of plaster fill to blend this correction of the forefoot into the arch. Requesting minimum fill maintains a tight, intimate contour that really supports the foot. The more plaster applied, the less control it provides because the addition of standard or maximum fill lessens the contact. Patients rarely reject devices with a lot of arch
fill because they feel good, but the therapeutic benefits are diluted. As a result, it is important to instruct the lab when you want minimum fill to
get a conforming cast with a good longitudinal arch. Conversely, certain rigid, non-correctable foot types do not tolerate full contact and need more fill and a lower arch. Over the last few decades with the proliferation of CNC milling, the manual task and art of cast balancing has shifted to software programs that intrinsically balance and post. These methods invert the foot to achieve the desired result and have the advantage of being both accurate and repeatable.
Posting
Extrinsic posting was originally introduced only to stabilize the rearfoot—not to apply an additional wedge. Adding a post strengthens the shell itself, limiting deformation, and provides a wider base for controlling rearfoot motion through midstance. Depending on the amount of control required, posts can be formed from a variety of materials. With direct milled polypro orthotics, the post is an inherent part of the shell, making them extremely durable and long lasting. Crepe posts of various durometers are frequently used to vary control, shock absorption, and permit bench-top adjustments. The post’s finished contour also affects function. Traditionally, posts are beveled slightly inward to accommodate shoe fit. Straight-walled posts, although wider, resist torque and offer more control of the rearfoot. Longer posts that extend distally toward the arch give more support. These are most often prescribed for pediatric orthotics where shoe fit is not such an issue and maximum control is preferable.
Skives
Another modification to exert rearfoot control is the Kirby heel skive. This technique removes plaster from the calcaneus of the positive mold. Shaving away 2mm, 4mm, or 6mm of plaster at an angle introduces pressure that increases the ground reaction force and enhances orthotic control. This shifts the influence of the orthotic toward the medial rearfoot. A medial heel skive is particularly effective for flexible feet that have a medially deviated STJ axis and helps patients with early-stage adult acquired flatfoot.
Accommodations
Drops and depressions, also referred to as sweet spots, can be provided in the shell of functional orthotics to accommodate bony anatomy, fibromas, and scars. For example, a well that contours a prominent base of the fifth metatarsal can significantly improve patient acceptance. Heel-spur pain can be lessened by cutting a hole in the heel and back filling it with a plug of PPT. A plantar fascia groove or channel can be formed in the orthotic shell to accommodate the medial slip of a prominent or tender plantar fascia.
First-ray cutouts come in a variety of shapes to improve the function of the first metatarsal phalangeal joint. The original Root design raised the base of the first metatarsal at the apex of the medial arch and completely removed the shell under the first metatarsal head. Modern variations remove less of the shell while still allowing the first metatarsal head to make full ground contact. Their disadvantage is that they narrow the shell under the forefoot, reducing support at a critical instant in gait. Similar results can be obtained without altering the shell width by using a Reverse Morton’s Extension. The uses and benefits of Morton’s Extensions are well understood and are discussed in “Morton’s Extensions,” The O&P EDGE, May 2018.
Forefoot modifications play an important role in the function of orthotics as the mechanical effectiveness of the shell diminishes once heel rise begins. Sulcus posting, the addition of flexible material distal to the shell, can alter the loads and mechanics of the forefoot in the second half of gait. Likewise, metatarsal pads, sesamoid pads, and toe crests, although not part of the functional shell, can play a significant role in the efficacy of the final device.
Conclusion
The first step in designing a functional custom foot orthotic is to recognize the underlying biomechanical dysfunction contributing to the patient’s pathology. By understanding the cause behind the diagnosis, each orthotic can be uniquely designed to alter or lessen the destructive forces rather than simply treating the symptom. The patient data will inform the final choices, and material selection, shell trimlines, cast modifications, and posting each play a role in the overall effectiveness. The combination of the subtle variations will affect the outcome. O&P EDGE
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
Resources
- Scherer, P. R, ed. 2011. Recent Advances in Orthotic Therapy: Improving Clinical Outcomes with a Pathology- Specific Approach. Lower Extremity Review.
- Chapter1: Prescription writing for pathology-specific foot orthoses. In Recent Advances in Orthotic Therapy: Improving Clinical Outcomes with a Pathology-Specific Approach.
- Valmassy, R. 1996. Clinical Biomechanics of the Lower Extremities, 1st ed. Mosby.
- Chapter13: Prescription writing. In Clinical Biomechanics of the Lower Extremities, 1st ed.