The objective throughout the series has been to provide general guidelines for the design of custom foot orthotics relating to specific conditions. This article focuses on some of the more common diagnoses encountered by clinicians treating pediatric patients.
For some practitioners, working with children can be rewarding because it is possible to visually monitor their improvements. More importantly, conservative orthotic care of younger patients, particularly before seven or eight years of age, can correct orthopedic abnormalities. This can circumvent the development of compensations that might otherwise be carried into adulthood, lessening the need for surgeries. In other words, proper early orthotic treatment can have benefits that last a lifetime.
Pediatric Flatfoot
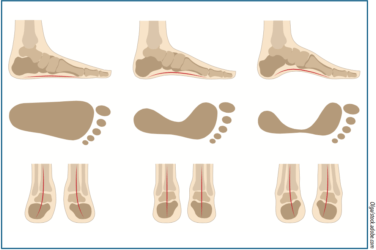
At present there are conflicting opinions regarding when it is appropriate to treat pediatric flatfoot. This is an ongoing conversation that shifts between early conservative intervention, and conversely taking a wait-and-see approach. However, there is much at stake. The foot of a newborn is encased in fatty tissue, and upon weight bearing there is almost always the appearance of a pes planus. This may not be a true flatfoot, although the arch is hidden in a bulbous shape. Usually, the calcaneus in infants is everted, but during normal development this eversion reduces by approximately 1 degree per year. Decisions made about children’s health during their critical early development may not be apparent for years or decades, and often the full results are realized only as adults.
It is important to recognize that not all pediatric flat feet are the same, and they can be categorized into sub-groups. The first major distinction is between rigid and flexible. A rigid flatfoot is one that remains flat during non-weight bearing and weight bearing. The foot shape is not correctable, and there is a significant limit or absence of motion. Rigid flat feet in children can result from many issues, including osseous coalitions or a vertical talus that require specific investigation and diagnosis. Physicians will evaluate, determine the cause, and treat these cases based on the patient’s age, prognosis, and surgical options. A second factor to consider is pain: the symptomatic versus the asymptomatic foot. Most physicians and parents will readily treat the symptomatic foot, especially if the child is avoiding activity to limit pain or discomfort.

However, addressing both categories still leaves the largest segment of the group—children with an obvious flatfoot but currently no discernible issues. With experience, skilled practitioners can learn to distinguish a flat foot, that is a foot with no arch or a low arch, from a developmental flatfoot condition. A low-arched foot may be properly aligned and not exhibit any signs of pronation. On the other hand, for children six years or under, a developmental flatfoot is one that demonstrates excessive pronation while weight bearing. Pronation is triplanar, and one may notice some or all of the following: navicular drop, medial prominence of the talar head, forefoot abduction, or a concavity along the lateral border of the foot. None of these signs should be considered normal.
Developmental flat feet appear normal when non-weight bearing but collapse once the child stands. It has also been referred to as a hypermobile foot, and it presents bilaterally. Unilateral presentation requires further investigation, and issues such as a leg length discrepancy should be considered. It is important to note arch height alone is an unreliable indicator, but excessive pronation is abnormal at any age. A full description of this foot type is detailed in a series of articles by Joseph D’Amico, DPM1.
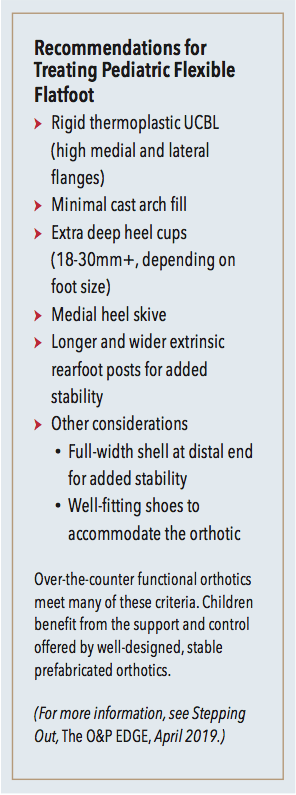
Although a child may be able to tolerate an everted foot position—presenting as asymptomatic—it is firmly believed that repetitive stresses acting on this vulnerable foot will lead to pathology. The decision whether to treat should be based on a thorough biomechanical examination. When working with children, it is always important to be aware of other systemic disorders and neurological conditions that may contribute to flat feet. The clinician must also check for equinus; pronation in young children can often be a compensation for a restriction in ankle motion. Foot orthotics are often prescribed for children with flexible flatfoot. The UCBL with extended heel cup walls is the classic pediatric foot orthotic design, offering rigid control.
Toe Walking
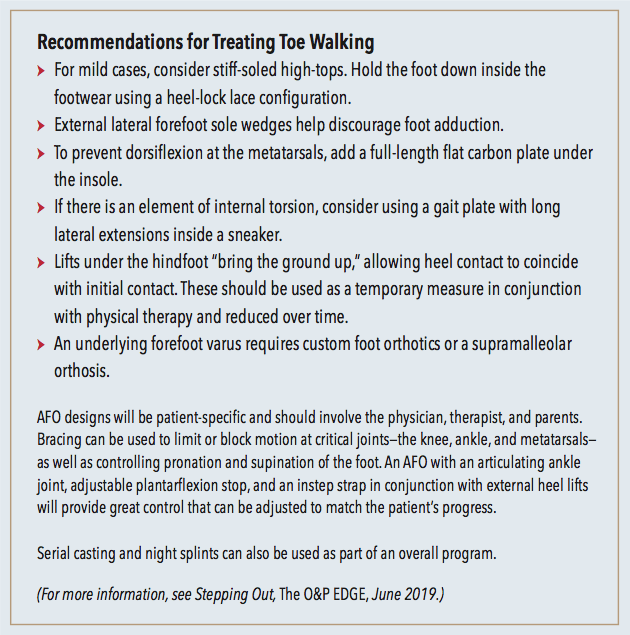
Toe walking is not considered part of the normal development of gait, but it is seen as a common variant that many children go through. It is not unusual that young children exhibit a brief phase of toe walking for three to six months and then outgrow it. If it remains persistent, it is important to investigate further. Recent research has looked at a host of factors such as patient motor sensory deficits, sensitivity to vibration, and a possible genetic link that may be contributing to this unique gait style.
There are several known etiologies of toe walking that are well documented. For example, an abnormal soleus or defects of the central nervous system that result in equinus may cause a child to walk without heel contact. Likewise, toe walking is one possible compensation for an Achilles contracture. Toe walking associated with other pathologies such as cerebral palsy, muscular dystrophy, and autism is more clearly understood, but researchers are beginning to focus on milder undiagnosed conditions that may also play a role. The list of more subtle factors to be considered includes neurodevelopmental impairment, vestibular dysfunction, attention-deficit/ hyperactivity disorder, issues with vision, or other forms of delayed development.

Given the array of possible serious contributing factors, idiopathic toe walking is diagnosed by exclusion, i.e., it is essential to first rule out any neurological or orthopedic causes. Examination includes an extensive medical and family history, a neurologic exam, and a thorough biomechanical and gait evaluation. This history includes assessing risk factors from birth, including birth weight, prematurity, or any other indications of physiological stress.
As part of the overall assessment, parents should be questioned as to when toe walking began and whether the percentage of time spent walking on the balls of the feet is generally decreasing or increasing. To rule out equinus, there should be at least 5 degrees of passive dorsiflexion with the subtalar joint held in the neutral position. The Silfverskiold Test can be used to check both range of motion and muscle spasticity. Patients with a fixed plantarflexion are unable to get their heels to the ground without severe compensation. The goal of treatment is to encourage a fluid and stable heel-to-toe gait, correct leg and upper- body positioning, improve balance, and prevent loss of range of motion—particularly at the ankle.
In-toe Gait
Up to the age of five or six, children usually demonstrate external limb rotation. As the child develops, there is a gradual rotation of the patellae towards the frontal plane. Any mild in-toeing should be noted as being within normal range, symmetrical, and decreasing over time. Asymmetry of either patellar or foot position may be an indication of an underlying issue.
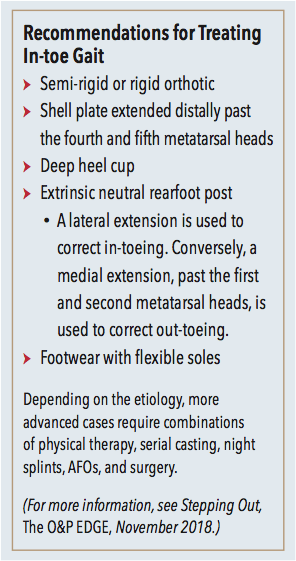
In the early years, the femur and tibia have inherent rotations due to a combination of torsion and position. Torsion of a long bone is an osseous abnormality referring to increased rotation about the longitudinal axis. Position of a bone describes the attitude of the bone as a result of soft tissue or muscular forces. Often torsion and position are present together, each playing a role influencing limb rotation. Torsion is structural whereas position is functional and may only appear when the child walks or runs.
Anteversion means “rotated forward” and refers to the orientation of the femoral neck and head in relation to the condyles at the knee. Typically, at birth there is a noticeable internal angulation, and this gradually reduces to 8 to 12 degrees in adults. Internally facing patellae indicate anteversion due to internal femoral torsion. However, if both patellae face forward on the frontal plane but the feet are adducted, then there is likely either internal tibial rotation or a metatarsus adductus. It is not unusual to see combinations of these factors present together. Metatarsus adductus is a common pediatric abnormality that responds well to early conservative treatment. Importantly, if missed or ignored, it can lead to problems later in life such as a prominent and painful base of fifth metatarsal, difficulty with shoe fitting, and perhaps early hallux valgus.
Foot orthotics can help address in-toeing, but their effectiveness depends on the level (foot, tibia, or femur) and extent of the deformity. In mild cases, an orthotic with an elongated foot plate alters the break in the shoe. It restricts motion at the lateral metatarsal heads, while the longitudinal arch support and deep heel cup prevent compensatory pronation.
Calcaneal Apophysitis
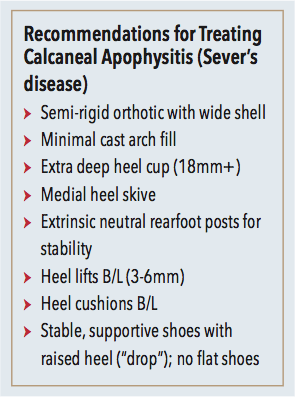
Apophysitis describes an inflammation or stress injury to a growth plate, and it is a common ailment in active adolescents. Calcaneal apophysitis, also known as Sever’s disease, refers to pain, swelling, and tenderness specifically at the heel. The attachment of the Achilles tendon makes this a vulnerable spot for children engaged in competitive sports, and they are particularly susceptible during growth spurts. Simple, effective cures include rest, icing, and limited stretching of the calf muscles. It is also beneficial to provide heel lifts to reduce strain, along with supportive shoes and insoles. The goal is to reduce tension on the posterior heel and most cases resolve with these measures.
Conclusion
Within the academic podiatric community, it is firmly believed that children with lower-limb abnormalities should receive early treatment to align their feet and limbs. As growth plates are still open and structures are not yet fully formed, orthotic interventions along with physical therapy can be used to influence both development and gait. Correcting rotations and limiting excessive pronation reduces destructive forces acting on the open, malleable foot. Children whose biomechanical metrics lie beyond the normal range should be monitored closely. If they are going to outgrow it, the practitioner must track consistent changes in the key indicators and ensure steady progress. If the abnormality remains persistent, proactive measures should be taken. Children go through a golden age where conservative treatment encourages normal development, setting them up for a lifetime of good exercise habits and pain-free walking.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.