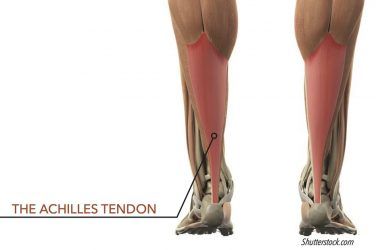
Adult-acquired flatfoot (AAF) is defined as a progressive deterioration of the static and dynamic structures that support the foot. Although frequently linked with posterior tibial tendon dysfunction (PTTD), AAF is a far broader syndrome that describes a gradual but painful breakdown of the weight bearing foot.
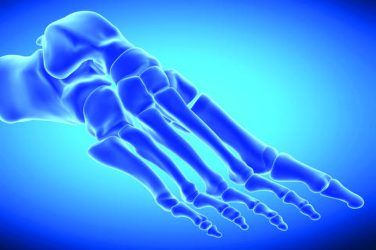
In a previous article, “Understanding Adult-Acquired Flatfoot” (The O&P EDGE, November 2014), we looked at some of the causes of this condition, which usually begins with bilateral pes planus, progresses to PTTD, and can ultimately end up as a fixed deformity with midfoot collapse and forefoot abduction. Along this trajectory, the foot moves through clearly defined stages as the key supporting ligaments are attenuated, midfoot joints become subluxed, and the foot becomes more rigid.
Several tests can be used to evaluate and stage AAF. The patient’s initial complaint will often be unilateral pain along the course of the posterior tibial (PT) tendon. It is helpful to recognize that, although the symptom may appear to be local, the effect on foot function is occurring in all three planes. For example, a lower arch due to PT muscle weakness can lead to a restriction of the critical first metatarsal phalangeal joint (MPJ) (sagittal plane motion). This, in turn, blocks the windlass mechanism, resulting in an unstable midfoot after heel lift, which is often seen as calcaneal eversion (frontal plane motion). Although not an exhaustive list, the spectrum of tests in this article will assess the loss of foot strength and function in several dimensions. Radiographic analysis and nerve conduction tests will confirm the extent of the condition.
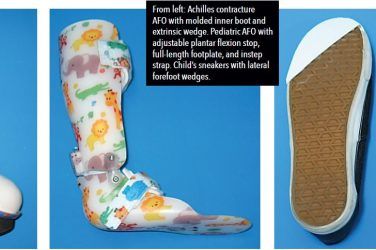
Given that AAF progresses in a somewhat defined pattern, there are appropriate treatment protocols to address each stage of the condition. The goal is to provide adequate support to prevent further pathology-without restricting beneficial motion. Thus, patients who exhibit the early stages of AAF can often be treated successfully with functional foot orthotics and physical therapy, whereas patients in the later stages require the more restrictive control of AFOs and perhaps surgery.












For a more complete review of the etiology and staging of AAF, read “Biomechanics and Clinical Analysis of the Adult Acquired Flatfoot,” Douglas Richie Jr., DPM, FACFAS, Clinics in Podiatric Medicine & Surgery, 2007.