Give me a lever long enough and a fulcrum on which to place it and I shall move the world.
-Archimedes of Syracuse
Human ambulation is a fascinating subject. Anthropologists claim that the evolution to upright bipedal locomotion was one of the most significant adaptations to occur in human development, and it sets us apart within the animal kingdom. Walking is something that most of us take for granted, but it is, in fact, a complex series of timed events. Smooth gait requires a precise and synchronized sequence of neuromuscular activity, joint motion, and gravitational reaction in order to progress fluidly and efficiently. Treating patients with gait-related pathologies requires a thorough understanding of normal walking and the mechanisms that may interrupt its subtle balance.
Walking has been called a sagittal plane activity. Clearly, all three planes are involved, but the greatest joint range of motion (ROM) and the line of progression occur in the sagittal plane. To maintain a flowing and steady forward motion, there is a critical dependence between all the major joints of the lower limb. We can appreciate that without motion at the hip, walking would be very difficult. Knee flexion is essential for ground clearance and forward progression without hip circumduction. Motion at the ankle joint allows the body weight to pass uninterrupted directly over the plantigrade foot. In midstance, the foot acts as a stable anchor to everything above it, and then rapidly transforms into a versatile hinge as heel lift occurs and the opposite limb swings forward. But there is one final joint upon which each of these depends. It is not surprising, if you follow the sequence of events from hip to knee to ankle, to recognize that the most distal joint can have the greatest impact on all of those above it.
The First Metatarsal Phalangeal Joint
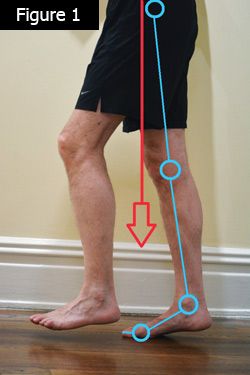
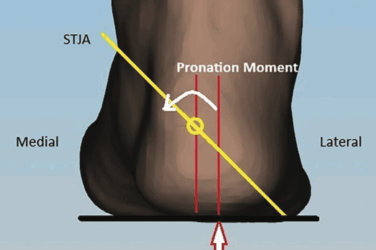
The operation of the first metatarsal phalangeal joint (MPJ) is immensely important, and it has tremendous influence on proper gait. During midstance, once heel lift begins, the full body mass rotates around the first MPJ (Figure 1). Its improper function may be the cause of a host of pathologies farther up the chain.
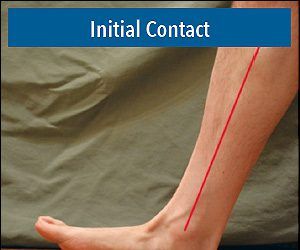
Once the heel strikes the ground and the foot proceeds to make full contact with the supporting surface, the hallux does not move forward again until swing begins. Prior to toe-off, the orbiting body advances in relation to the immobile forefoot in what is referred to as an inverted pendulum. The talocrural joint at the ankle accommodates some of this arc, and the tibia may reach 10 degrees of dorsiflexion (DF) in relation to the foot, but the momentum of the body pulls it further, initiating heel lift. If the forefoot is to remain in contact with the ground, the remaining ROM needs to come from the first MPJ.
Any block in motion at the first MPJ directly affects more proximal joint motion. When it is restricted, it can lead to a variety of compensations as the body naturally seeks alternative paths to continue forward motion. The result can be pathologies such as neuromas, Achilles tendon pain, or knee arthritis-all of which are remote from the first MPJ. One possibility is to rotate the leg externally so that body weight passes over the side of the foot rather than along its long axis. A blockade in the action of the first MPJ also inhibits the operation of the windlass mechanism. The windlass is the effect created when the hallux is dorsiflexed in relation to the foot, automatically pulling the plantar fascia (PF) taut to “close pack” the bones of the medial arch. If the windlass effect is inhibited, there is no tension on the PF and the bones of the midfoot are left “loose” at a critical point of gait. This often results in symptoms associated with late-stage pronation such as pes planus, plantar fasciitis, and heel pain. A true block of first MPJ motion can also have the effect of interrupting the completion of each step. Every time the momentum of the body weight is halted, however briefly, that energy gets dissipated into the trunk, contributing to a downward tilt of the head and slouched posture.
Early toe-off, in which the leg is lifted into swing and leads to a shorter stride, may also occur. This is tiring and less efficient because the natural momentum is lost at the end of each step. Dananberg describes this in detail, explaining how functional loss of motion at the first MPJ leads directly to lower back pain.1,2 Essentially, for smooth and efficient gait to occur, the thigh needs to reach a sufficient degree of extension. This helps momentarily stretch the muscles before they recoil, helping to accelerate the leg forward. If thigh extension is limited in any way, then the iliopsoas (IP) group must initiate rather than continue hip flexion. Now the muscles must fire to lift the leg. Repeated firing leads to fatigue and constant strain on the lumbar spine, which is the origin of the IP group.
Motion of the hallux and function of the first MPJ should be a key component of every biomechanical exam. The simplest test is to check for hallux ROM with the patient seated. Typically, in a non-weight bearing foot you would expect to observe 55 to 70+ degrees of DF. Limited motion in this open-chain test indicates a structural hallux limitus. The more severe hallux rigidus is a syndrome with symptoms that are related to degenerative arthritis of the great-toe MPJ. This may be dealt with surgically or by prescribing shoes with pedorthic modifications and custom orthotics.

Functional hallux limitus (FnHL) can be deceptive as it appears asymptomatic at the first MPJ and the patient can have full ROM in non-weight bearing open chain. The restriction occurs only during gait when the joint is loaded in closed chain. Clough3 describes a simple test where the foot is held in dorsiflexion and maximally pronated (Figure 2). The thumb is used to apply load under the first metatarsal head, displacing and elevating the medial column. The opposite thumb then attempts to dorsiflex the hallux. In a foot with FnHL, there will be a distinct lack of plantarflexion of the first metatarsal head and a perceived locking of first MPJ motion. Restriction of hallux motion under this scenario indicates FnHL during gait. If the hallux resists bending during activity, you may see altered wear patterns inside the shoes. Inspection of the sock liner can reveal an absence of wear under the first metatarsal and indications of more pressure under the great toe and lesser metatarsals.
Orthotic Treatment
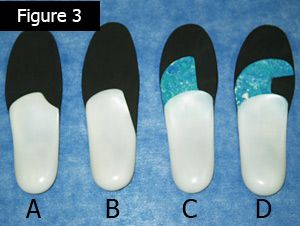
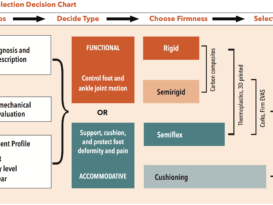
Accommodations to foot orthoses to improve function of the first MPJ and mitigate the effect of Functional Hallux Limitus: (a) Notch-style first ray cutout; (b) Root-style first ray cutout; (c) Reverse Morton’s extension; and (d) Kinetic wedge.
Patients with FnHL demonstrate good ROM in open chain. The blockage occurs as a result of misalignment of articular surfaces of the joint that jam when the foot is weight bearing and pronated in midstance. This gives a clue as to how orthotic design may restore some of the lost motion. Due to joint articulation, plantarflexion of the first metatarsal is necessary beyond a certain range for full hallux DF to occur. A well-fitting, custom foot orthotic will raise the medial longitudinal arch, support the midfoot, and maintain the first metatarsal in the proper, sloped alignment. In addition, accommodations can be made to allow the first metatarsal head to sit lower, further enhancing the bone’s angle of declination (Figure 3). A first ray cutout in the orthotic shell slightly drops the first metatarsal head. This is part of the Maximum Arch Subtalar Supination (MASS) Position Theory proposed by Glaser.4 Likewise, a reverse Morton’s extension provides a channel into which the first metatarsal can sit. Another option is to incorporate a kinetic wedge into the device. This is a rectangular-style cutout in PPT or EVA, distal to the orthotic shell, creating a depression for the first metatarsal. All of these approaches allow the first metatarsal head to drop down, and they also serve to transfer some of the forces laterally. Another technique is to preload the hallux by applying a slight distal wedge under the great toe. This modification is easily applied and has the advantage of engaging the windlass mechanism, although it may cause some rubbing inside the toe box of certain shoe styles.
Archimedes’ lever may well have been capable of moving the world, but it would only work if nothing impeded the motion of the lever upon that fulcrum. FnHL is an unsuspected block in the forward motion of the body and can result in foot pathology, altered gait, lower back pain, and even poor posture. Unrestricted operation of the first MPJ should be a critical part of every biomechanical exam and a consideration in orthotic design.
References
- Dananberg, H. 1993. Gait style as an etiology to chronic postural pain. Part I functional hallux limitus. Journal of the American Podiatric Medical Association 83(8):433-41.
- Dananberg, H. 1993. Gait style as an etiology to chronic postural pain. Part II postural compensatory process. Journal of the American Podiatric Medical Association 83(11):615-24.
- Clough, J. 2009. Functional hallux limitus: Diagnosis and treatment. Lower Extremity Review, October.
- Glaser, E., D. Bursch, and S. J. Currie. 2006. Theory, practice combine for custom orthoses. Biomechanics13(9):33-43.