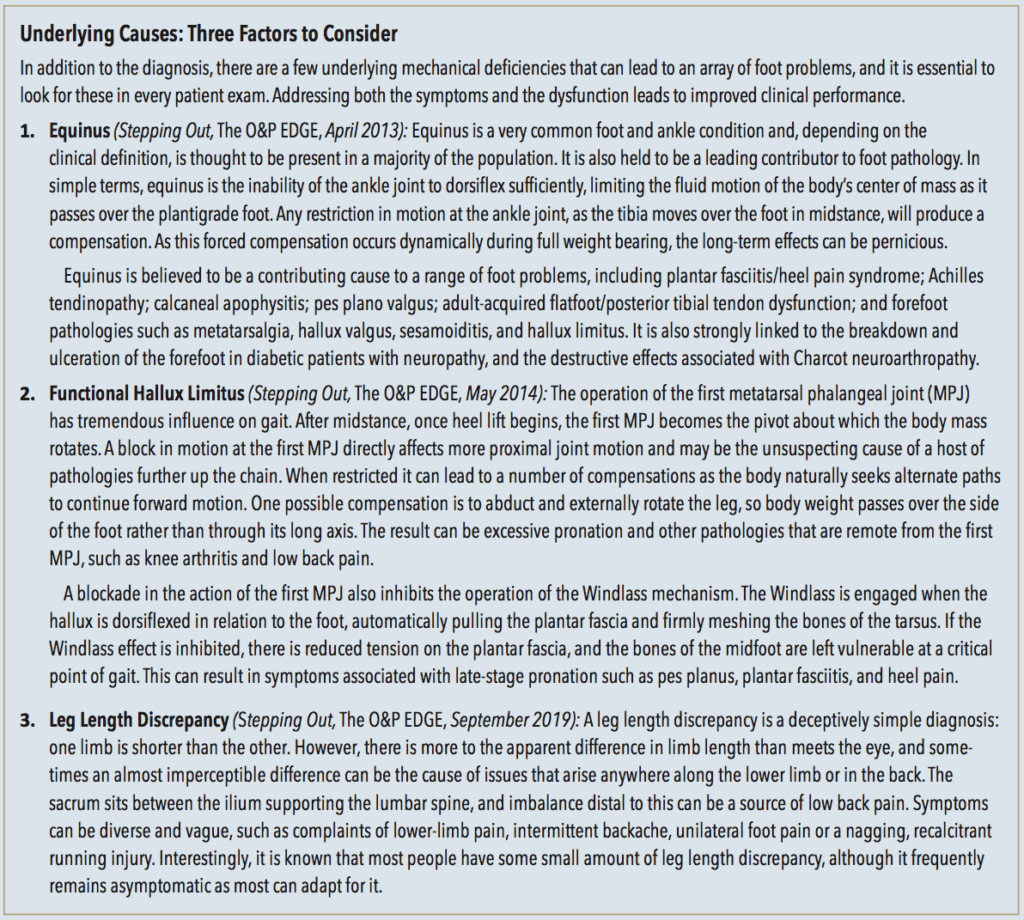
Clinicians who regularly see patients for custom foot orthotics are used to working with a wide variety of physicians’ notes. Sometimes they will be very precise, specifying the material, the exact degrees of posting, shell accommodations, etc. However, many prescriptions tend to be vague. They might include a diagnosis such as plantar fasciitis and mention little else except perhaps indicate the type as “functional.” A personal favorite is “foot pain—orthotics.” Although open-ended prescriptions can be challenging for newer practitioners, they are also opportunities to create the most effective devices. Fortunately, dispensing foot orthotics is a well-established science with a substantial body of research to guide the design.

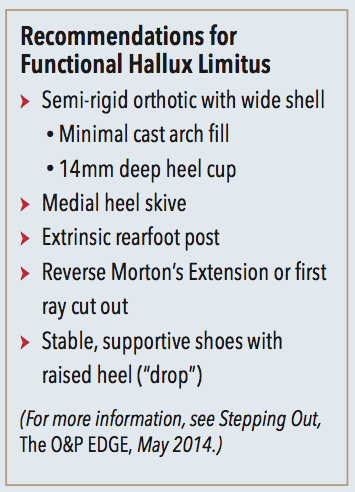
Functional Hallux Limitus
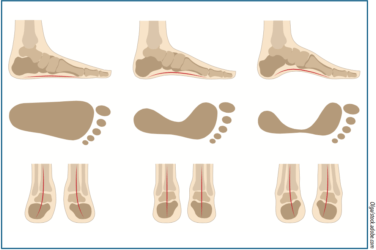
Transition to terminal stance and the third rocker literally hinges on the smooth operation of the first MPJ. The simplest test to check for hallux range of motion (ROM) is with the patient seated. Typically, in a normal non-weight bearing foot there will be 50-70+ degrees of dorsiflexion. Then, with the patient standing, elevate the hallux and note the available ROM. In a weight bearing foot with functional hallux limitus there is a distinct locking of the first MPJ motion. ROM of less than 12 degrees indicates functional hallux limitus. If the first MPJ resists bending during activity, you may even see altered wear patterns inside the shoes. Inspection of the insole can reveal increased pressure under the great toe and lesser metatarsals and an absence of wear under the first metatarsal head.
A block of the first MPJ motion has the effect of interrupting the completion of each step. Early toe-off may occur—where the leg gets “lifted” into swing—leading to a shorter stride. This is a tiring and less efficient gait as the natural momentum is lost. In some cases, it is thought to lead directly to low back pain as the muscles innervate to lift the leg. Repeated firing leads to constant strain and fatigue on the lumbar spine. Action of the first MPJ is improved by plantarflexing the first metatarsal bone. Orthotics that fully support the midfoot and lower the first metatarsal head enhance its motion.
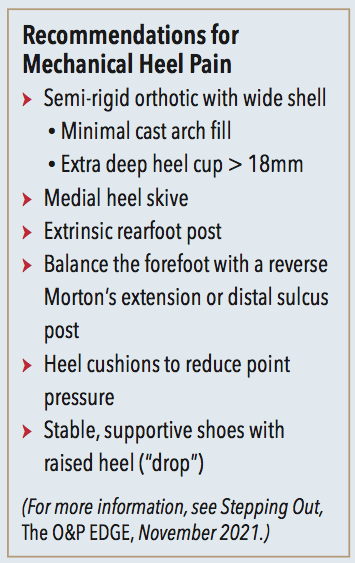
Mechanical Heel Pain
Heel pain is one of the most common reasons people seek medical care for the foot and ankle. It is also very treatable and numerous studies demonstrate the success of conservative measures such as foot orthotics, physical therapy, and taping. As there are many possible causes of heel pain, a careful diagnosis is essential to appreciate each of the contributing factors.
Plantar fasciitis is reported as the most frequent cause of heel pain, and the leading symptom is a deep tender pain that sometimes radiates into the arch. There is often pain along the fascia and in particular at the medial calcaneal insertion. Heel spur is another popular term used to describe the condition, however not all patients with plantar fasciitis develop calcaneal spurs. Other conditions that cause pain in the heel need to be ruled out, including nerve entrapment (Baxter’s neuropathy), calcaneal stress fractures, tarsal tunnel syndrome, and fat pad atrophy.
Heel pain that is mechanical in origin potentially has a mechanical solution, and research clearly shows the benefits of orthotic therapy in treating plantar fasciitis. A well-fitting and comfortable semi-rigid orthotic, suitable to the patient’s lifestyle, can be essential to healing the condition. In principle, an orthotic that inverts the rearfoot and adducts the forefoot reduces stress in the plantar fascia. For example, for patients with an everted foot, consider some combination of good medial arch support, extrinsic rearfoot posting, and a medial heel skive. The relative position of the forefoot can be accommodated with distal extensions such as a sulcus post or a reverse Morton’s. Deep heel cups (> 18mm) are used to limit calcaneal fat pad displacement and provide more rearfoot control. Equinus, often a contributing component, can be addressed with heel lifts, which should be dispensed bilaterally to avoid creating a leg length discrepancy. In cases where the medial aponeurosis is inflamed and tender, a plantar fascia groove may provide some relief.
Some patients respond well to the addition of heel cushions or heel spur cut-outs. The padding relieves point pressure and helps by elevating the heel. It is also important to consider the shoes that will be worn. Supportive shoes with a removable inlay, firm counters, and heel-toe drop or off-set of 10-12mm provide a good foundation for an orthotic device. In the case of runners, if there are signs of obvious wear or midsole compression, advise them to get new sneakers. It is recommended the midsole not be too soft, but the shoe itself should flex at the met heads. Stiff-soled shoes prevent dorsiflexion of the hallux and digits inhibiting the synergistic action of the Windlass mechanism.
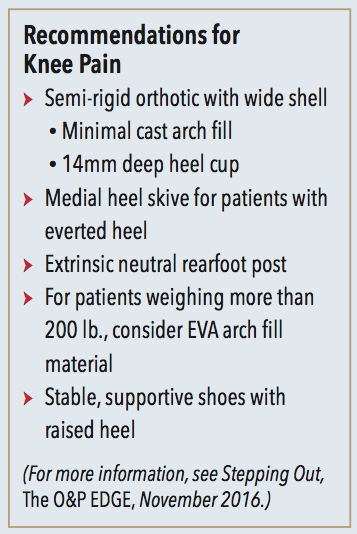
Knee Pain
Although exact numbers are difficult to determine, mechanical knee pain accounts for a significant portion of exercise and running-related injuries. There is no doubt knee pain is a complex subject, and even the leading researchers have more than one theory of etiology. Among these it is proposed that some mechanically induced knee pain has its origin in the biomechanics of the lower limb.
When a patient demonstrates foot pronation late in the gait cycle, failing to re-supinate appropriately, the resulting knee valgus puts a strain on the tendons and ligaments, potentially altering patella alignment. It is believed, though not universally accepted, that the torque from knee rotation and abduction may be the cause of pain. Foot orthotics and physical therapy can address some of these characteristics by properly supporting the foot, adjusting the timing and duration of pronation, and strengthening the muscle groups involved. Not all patients respond to these interventions, but it is possible to quickly test their potential by using combinations of prefabs, taping, and sole wedges. This also informs the design of the orthotics if they are seen to be helpful.
Lateral Ankle Sprain
Ankle sprain occurs when there is a sudden twisting of the ankle leading to pain, swelling, and loss of activity. The stresses from a forceful inversion and the loss of balance result in damage to some of the lateral ankle ligaments. Chronic ankle instability is recognized as repetitive bouts of lateral ankle sprain resulting from an inherent weakness in the ankle structure. Unfortunately, there is ample evidence that ankle sprain protocols are sometimes rushed, and poor initial treatment, combined with other factors such as age, lead to ongoing ankle weakness.
Functional instability refers to neuromuscular or proprioceptive deficits diminishing control. Mechanical instability describes a loss of the intrinsic stability of the ankle. This may occur from overstretched ligaments that become lax after a significant sprain. It can also indicate restricted ROM in the joints of the ankle or foot. The role of each overlaps, and it is believed that a combination of both are at work when patients repeatedly injure their ankles.
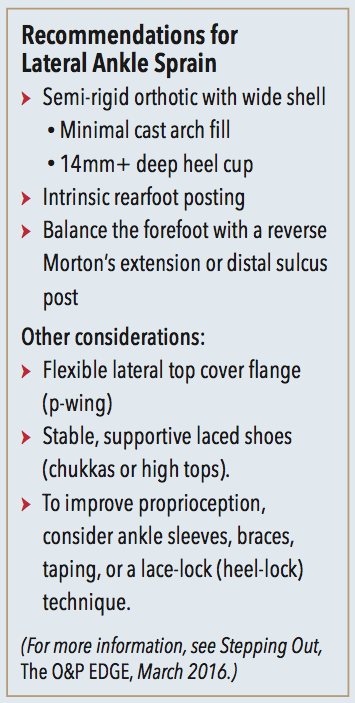
If forefoot alignment is one of the mechanical factors contributing to ankle sprain, then custom foot orthotics can be used to address the imbalance. When the weight bearing foot is inverted, there will usually be increased pressure along the lateral border. Rather than “push” the foot medially with a lateral wall, the use of forefoot posting, distal to the metatarsal heads, can rebalance forces. For example, in the case of forefoot valgus consider using a lateral wedge (from the fifth to third metatarsal) and extend it to the sulcus. Similarly, a plantarflexed first ray would benefit from a reverse Morton’s–type depression that elevates the sulcus of the forefoot from the second through fifth metatarsal. In both cases you are rebalancing the position and forces acting on the forefoot.
In combating chronic ankle sprain, the role of foot orthotics is to improve body position and allow greater range of motion. In the past it was thought holding the foot vertical was best and, as a result, many foot orthotics were extrinsically posted to neutral. With current understanding of the importance of postural control and the effect of pressure sensors on the plantar foot the role of orthotics has changed.
Foot orthotics should be designed to reduce strain on the foot, improve ROM, and enhance sensory feedback. Surprisingly these orthotics should not have a rearfoot post as this restricts motion of the sub-talar joint. An intrinsically balanced semi-rigid shell with a deep heel cup will improve plantar contact and give good mechanical support without blocking motion. Medial arch support and full-length cushion-top covers have the advantage of activating sensors along the entire sole. Distal sulcus posting can be applied to reduce internal compensations and rebalance the forefoot.
Recommendations for other common foot and ankle pathologies will be discussed in future articles.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.