“Think of the magic of that foot, comparatively small, upon which your whole weight rests. It’s a miracle, and the dance is a celebration of that miracle.” -Martha Graham
Although much of our time is spent addressing the symptoms and pathologies of pes planus, there is a significant incidence of pes cavus within the general population, with estimates ranging from 8 to 15 percent. As practitioners, we may not encounter high arched feet quite as frequently as other foot concerns, but it is important to understand the unique characteristics and treatment options for this foot type. This is all the more important because it appears that a majority of the patients who are classified as having cavus feet will experience foot pain.
Recognizing Pes Cavus
In the absence of pain it is possible to overlook the architecture of this foot type that may eventually lead to more severe conditions. One of the reasons that pes cavus garners less attention is the lack of a standard definition. It is generally recognized as a foot with an abnormally high arch, but mild forms can be asymptomatic and fall within the normal band of function. A cavus foot can be readily identified from a pedigraph imprint: There will be no ink under the medial arch and obvious weight bearing along portions of the lateral border. Pressure maps sometimes demonstrate the classic “tripod” characteristic of cavus feet showing a concentration of weight bearing at the first and fifth metatarsal heads and at the heel. This clear imprint of high-pressure spots can also serve as a basis for orthotic treatment.
Diagnosis can also be verified by lateral radiographs, which reveal critical angular relationships of the foot and ankle. The first metatarsal-talar (Meary’s) angle and the calcaneal inclination-first metatarsal (Hibb’s) angle can confirm when bone angulation is beyond the normal range.
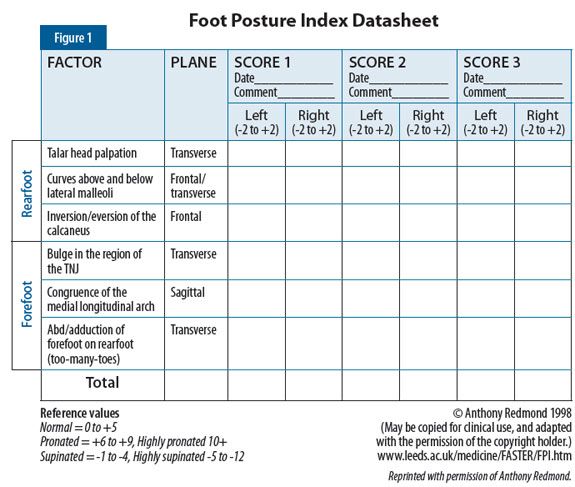
In the 1990s, the Foot Posture Index (FPI) was developed to classify foot type easily and reliably. This is a quick and effective protocol that clinicians use to grade each foot across six separate criteria. The patient stands still, in double-limb support, in the relaxed stance position. Each of the six component tests is simply graded: 0 for neutral, a minimum score of -2 for clear signs of supination, and up to +2 for pronation (i.e. positive scores equal pronation). The result is totaled and will fall within the range -12 to +12. Normal feet score 0 to +5, supinated feet are considered -1 to -4. Scores <-5 are classified as highly supinated. A more complete description of the method and additional copies of the data sheet displayed in this article are available at studylib.net/doc/8078879/the-foot-posture-index (Figure 1).
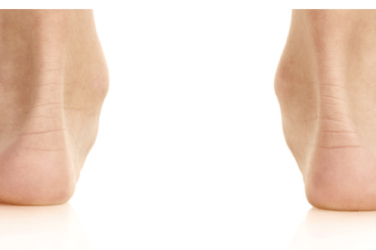
Another clinical indication of pes cavus, the “peek-a-boo heel,” is described in a 2005 paper by Manoli and Graham (“The Subtle Cavus Foot, ‘the Underpronator,’ a Review,” Foot and Ankle International). With this sign, the medial heel pad can be seen easily when looking straight-on from the front with the patient standing and the feet aligned directly ahead. In normal feet, the heel pad will not be visible since it lies behind the rearfoot. Although not a definitive test, if the medial heel pad is visible, you should suspect the presence of some degree of cavus. This can be confirmed by looking at the foot from the rear to determine heel varus.
Other indications of the presence of pes cavus include the nature of the symptoms presented, such as metatarsalgia-type pain and callusing under the ball of the foot, pain along the lateral column of the foot, lateral ankle instability and recurrent inversion sprains, plantar fasciitis, and stress fractures of the lesser metatarsals.
Etiology
Although the origins of pes cavus are not completely understood, there is a growing body of evidence to suggest it is a progressive deformity resulting from biomechanical imbalances. First, muscle strength inequality can come about due to a structural or anatomical deformity. The result can be an increased lever or moment, creating a mechanical advantage for a particular muscle group. It is vital that muscle groups work in harmony with their antagonists. Second, the imbalance may arise from a muscular deficit. Neuromuscular disease can be congenital, genetic, acquired, or idiopathic. For example, it is common to see pes cavus associated with conditions such as congenital clubfoot, Charcot-Marie-Tooth disease, muscular dystrophy, and post-polio syndrome.
Regardless of cause, the result is an imbalance in the foot that allows one muscle group to overpower another and slowly influence foot architecture. Under this scenario, the foot is seen as being gradually pulled into cavus. The underlying cause may be multifactorial, and the physician needs to conduct a thorough medical exam and history, biomechanical exam including gait analysis, and motor function tests to determine the true origin and generate a treatment protocol.
In his latest book, Recent Advances in Orthotic Therapy, Paul Scherer, DPM, MS, devotes a full chapter to pes cavus. In it, he describes a theory of the developing pediatric foot as a delicate balance of support structures made up of functioning muscle groups, antagonists, and precise lever arms. He proposes that equilibrium disruptions lead to imbalances and increasingly permanent alterations in foot morphology.
Classification
Pes cavus can be separated into several categories.
 An example of a pes cavus foot type.
An example of a pes cavus foot type.
Anterior cavus is recognized as a plantarflexed forefoot in relation to the rearfoot. This can be seen most clearly in lateral radiographs: The rearfoot appears normal, there is a characteristic bump on the midfoot, and only the forefoot angles or drops downward. The cavus foot compensation for this “forefoot equinus” is to dorsiflex at the ankle joint. This creates the high arch. Over time it progresses, bringing the rearfoot and forefoot closer together, eventually becoming more rigid as ligaments contract.
Posterior cavus occurs when the rearfoot presents with a dorsiflexed subtalar joint (STJ) as viewed from the sagittal plane. It is often the result of a weakened triceps surae muscle group. Without an opposing pull, the dorsiflexors dominate. This can lead to a more vertical calcaneus drawing of the forefoot against the rearfoot, leading to an increased global deformity.
In either case, the consequence is reduced ground contact area. Muscle imbalance leads to digital clawing and increases pressures locally, manifesting as callusing on the metatarsal heads and also hammertoes. The Coleman block test is a simple technique to determine the nature and involvement of the cavus foot. Begin by observing the patient from the rear and note the level of heel varus. Then have the patient stand on a raised platform or block with the hallux and first metatarsal dropping over the medial edge (Figure 2). If the first metatarsal drops below the plane of support and the amount of heel varus is partially or completely corrected, then you can assume that the STJ has available range of motion (ROM) and a plantarflexed first metatarsal is contributing to the condition. This is a variation of anterior cavus where, as compensation, the dropped first metatarsal is forcing the rearfoot into varus. In this case, consider using a foot orthotic with a depression for the first metatarsal or, if space permits, building up the forefoot under the second through fifth metatarsals.
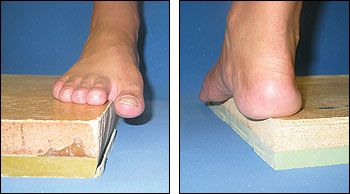 Figure 2: The Coleman block test.
Figure 2: The Coleman block test.
Treatment
A cavus foot with some motion available at the STJ allows for partial compensation and may be treated in a variety of ways. Compensations can also occur at the midtarsal joint or farther up the chain at the ankle and knee. More rigid feet, which remain uncompensated, may need very specific custom shoes, foot orthotics, or surgery to alleviate the symptoms and pain.
Typically, physicians prescribe accommodative orthotics for this foot type. Any total-contact orthotic that cradles the plantar foot and helps distribute pressure evenly across the entire surface will be beneficial. Using softer EVAs and foams can help replace shock absorption that is often lacking, but thermoplastic devices that make full contact also work well. Plaster casts should be prepared with the minimum amount of arch fill necessary to “bring the ground up to the foot,” and the orthotic should be wide enough to encompass the full width of the foot. Depressions or drops relieve specific areas of pressure, which are often indicated by the presence of calluses. Wide, cushioning metatarsal pads or bars will relieve pain and redistribute loads away from the metatarsal heads. Cushioning top covers such as those from Spenco or an under layer of PPT are also an excellent choice if there is sufficient room inside the shoe.
Orthotic posting will depend on the primary site contributing to the deformity but should only be prescribed based on the available ROM. A wide, neutral rearfoot post will increase the lateral ground reaction force at heel strike. Deep heel cups will also help control the tendency toward inversion. Patients with an anterior cavus essentially have a dropped forefoot, which can sometimes be offset by a heel raise extending to the mid arch.
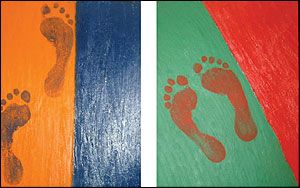 The high arched feet in these paintings demonstrate a similar pattern to the pediagraph imprint of a pes cavus foot.
The high arched feet in these paintings demonstrate a similar pattern to the pediagraph imprint of a pes cavus foot.
In general, cavus feet require well-fitting shoes with plenty of room for the high instep. Many of these feet present with a characteristic bump on the dorsum, which is easily irritated by the shoe tongue and closure. Blucher-type shoes with padded tongues are often the best choice. There are clever pedorthic lacing techniques that allow the tongue to expand around the boney prominence. Shoes with nonrigid toe box material and good toe height are also beneficial as individuals with cavus feet often develop hammertoes. Lateral wedges can be added to the midsole of some shoes to improve control. Lateral flares provide a wider base of support and can resist ankle torque.
In more severe cases, shoes may incorporate lifts for equinovarus-type conditions or leg-length discrepancies, and custom shoes can be constructed with long and high lateral counters. Likewise, short, articulating AFOs or leather ankle gauntlets can be prescribed to control inversion sprains.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York, New York. He can be contacted at seamus@hersco.com or by visiting hersco.com.