An ounce of prevention is worth a pound of cure,” is a saying attributed to Benjamin Franklin. When it comes to neuropathy, this is certainly great advice. The presence of, or potential for, any form of neuropathy in a patient must be given full attention. It is the signal that serious foot complications may not be too far away and could arise at any time.
Neuropathy
Neuropathy in its simplest form is nerve damage. The word is derived from two parts: “neuro,” referring to the nerve, and “pathy,” indicating disease. Many people can develop neuropathy, which is basically the loss of full sensation of nerve endings. Nerve function may be impaired due to trauma, genetic conditions such as spina bifida, alcohol abuse, and many other diseases.
 |
| Solid Ankle Foot Orthosis (AFO), Plastazote® lined. |
Peripheral nerves are the nerves that extend outside the brain and spinal cord. There are three types of peripheral nerves: motor, sensory, and autonomic. Motor nerve fibers carry signals to muscles to allow motion. Sensory nerves carry information to the brain about our environment (e.g., texture, warmth, or pain) from sensors in the skin and from deep in the body. The autonomic nerves are those that are not consciously controlled, such as those that control the bladder or pace of heart beats.
The most commonly seen peripheral neuropathy is a result of the complications from diabetes. Diabetic neuropathy is directly related to the length of time that nerve fibers are exposed to hyperglycemia. Elevated blood glucose levels will over time decrease nerve function. Loss of function such as weakness or decreased feeling and symptoms of prickling, tingling, or pain may occur together. Loss of sensation begins a cycle where damage can occur to the skin. Loss of feeling usually starts at the extremities (distal neuropathy), in the hands and feet, so particular attention needs to be paid to any wounds or lesions that may develop there.
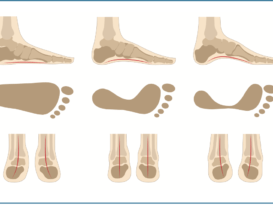
Motor neuropathic changes can manifest as involuntary muscle contracture. The effect on the feet can be seen as a clawing of the digits. This can lead to increased pressure on the plantarflexed met heads, which can be especially troublesome if there is an accompanying anterior migration of the plantar fat pads. This sets up a situation where there is increased pressure on the met heads, no fat pad to absorb shock, and no perception of pain. Repeated cycles of stress under these conditions will lead to breakdown of the skin.
One of the difficulties in treating patients with neuropathy is that as a result of the lack of sensation, they may be doing damage to themselves and not really feel it because of the diminished response from the nerves. In addition, once damage is done, the healing process is often impaired with these patients-making the recovery much slower. Due to the repetitive stresses and constant weight on the feet during walking, the foot is the number one site for ulceration for patients with peripheral neuropathy. It also is very difficult to heal these foot ulcers, as most patients want to remain active and prefer not to sit around waiting for wounds to close.
This is a very simple overview but it expresses the concerns that all healthcare providers have to: a) prevent neuropathy if at all possible, and b) immediately treat any skin callusing or potential for breakdown once neuropathy is present.
Charcot
One of the more advanced complications of neuropathy in general occurs when the joints of the foot begin to break down. This is more commonly known as Charcot’s joint disease. Although it occurs in only a small percentage of the diabetic population, it is a debilitating condition that needs to be treated aggressively if amputation is to be avoided. Several theories on this joint destructive process have been advanced, but the beginnings of the disease are not yet fully understood. It is accepted that there are many factors that lead to the condition.
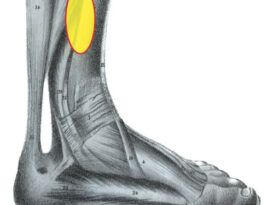
The primary components leading to Charcot neuroarthropathy are the existence of neuropathy and some trauma. This can start the cycle of degenerative joint disease, osteolysis around the joints, and ligament laxity and often is accompanied by increased blood flow to the foot. In the early stages, a patient with neuropathy in both feet may notice swelling on one foot; there also may be an elevated foot temperature.
Due to the presence of neuropathy, the initial onset of Charcot may or may not be accompanied with foot pain. The breakdown in foot structure usually occurs in the midfoot. This leads to prominent bone displacement, or subluxation, which often creates areas of localized high pressure on the skin. Once this begins, it is essential to try to off-load the high-pressure locations and redistribute the weight evenly across the entire bottom of the foot. In advanced cases, removing all weight bearing from the foot may be necessary.
Charcot deformity is classified in several stages:
- Stage I: Developmental or “hot” phase. Presence of hyperemia and edema, joint subluxation, dislocation, debris formation, and bony fragmentation.
- Stage II: Coalescent phase. Debris absorption, sclerosis of bony ends, and coalescence of bone fragments.
- Stage III: Remodeling phase. Marked decrease in swelling. Decreased sclerosis, remodeling of bony fragments, and fragments fusing to the joint surfaces in an effort to recreate the architecture of the foot.
- More recently, a Stage 0 has been described as ranging from a clinically warm, edematous, and painful foot to one with mild fracture or joint space widening (without debris).
Early detection at Stage 0 will greatly limit damage and can be treated with conservative measures. The most basic treatment is to get proper fitting shoes that will accommodate the swelling and allow adequate room for protective foot orthotics. Good shoes will include the following features:
- Firm heel counters and uppers to help control the foot in the shoe and prevent excessive motion and rolling.
- A firm and possibly wide outsole to provide a stable base for the foot.
- Extra-depth construction with a removable inlay that gives added cushion. This inlay can be removed to allow room for a custom foot orthotic if prescribed.
- Sometimes prescribing stiff-soled shoes with full-length steel shanks, or adding carbon plates, will help reduce pressure on the forefoot.
In cases where the swelling has progressed too far, it may be necessary to buy two different sized shoes of the same style. The alternative to this is to consider custom-molded shoes which are made individually from plaster casts of each foot and include their own custom insoles.
Full-foot custom-molded orthotics can be made with reliefs for the areas of high pressure. The right choice of materials will provide cushioning, reduce shearing friction, and protect the skin from breakdown. They also will help control the foot position and reduce excessive pronation. Accommodative foot orthotics are made from a variety of materials such as EVAs, Thermocorks®, or leather. Prescribing deep heel cups and sometimes high medial flanges will help cradle the foot for maximum stability. Foot orthotics with soft top covers will protect the skin. Plastazote® is often the first choice but it needs to be refurbished frequently, before it wears down excessively.
Correct management of Charcot joint disease requires constant vigilance and frequent checkups by a podiatrist or other qualified expert. They will evaluate the effectiveness of current shoes and orthotics; inspect the integrity of skin; note changes in the size, shape, and temperature of the feet; address the presence of any calluses forming on the skin, etc.
If the disease advances to the later stages, treatment will become more aggressive. All over the country, wound clinics have become the specialists in treating and healing stubborn ulcers. Some of the options available include one or more of the following:
- Prescribing an AFO to off-load the bottom of the foot and control the motion of the foot and ankle. There are many types and styles of AFOs that may be used depending on the level of control and off-loading required.
- Providing total contact casting (TCC) to fully transfer all of the weight away from the surface of the foot. This is a time-consuming but effective modality.
- Insisting on full and complete rest for the patient to allow the wound to close. This often proves difficult to achieve.
- Performing complicated surgeries to rebalance and/or fixate the foot, including external fixations or bone fusions.
In addition there are a host of specialized wound medicines and techniques available to promote the growth of healthy skin and limit infections, such as skin gels, growth factors, and topical antibiotics.
Partial Amputation Toe Fillers
 |
| Left: AFO with Plastazote® lining; Right: Custom insole with partial foot amputation toe filler. |
Sometimes, despite the best of intentions and efforts, nothing can be done to prevent the advancement of wounds and ulcers. In order to limit further and far more serious complications, such as gangrene, the best option is to amputate. There are many considerations involved as to the level of an amputation and it will depend on variables such as a patient’s weight, activity level, vascular system integrity, presence of healthy tissue, etc. Some amputations may require a prosthetic device, but many foot amputations will remove only a particular small aspect of the foot or perhaps a single digit.
Although partial amputations do not usually require prosthetic devices, patients can benefit from a toe filler that mimics and replaces the part that has been removed. Good fillers may allow patients to continue wearing their existing wardrobe of footwear, and cosmetic acceptance can often be a big part of getting beyond the surgical loss. Without a toe filler, the foot may have too much room and slide inside the shoe, or the upper may crumple or collapse at the site of the missing digits. Toe fillers can be made from a variety of materials such as EVAs, corks, or Plastazote, and often are incorporated onto custom foot orthotics. They then can be moved from shoe to shoe. If the level of amputation is more severe and whole aspects of the forefoot have been removed, then custom shoes may be required. They can be designed with matching shapes for the shoe fronts. They also may need stiff soles and rockers to prevent excessive bending of the shoe during the stride.
Neuropathy is a very serious condition that can lead to Charcot joint disease and possibly amputation. Paying full attention to foot health is one more way to help ensure a patient’s continuing active and full life, and avoid some very costly consequences.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.