Tarsal tunnel syndrome (TTS) was first recognized in the early 1960s and described as “pain in the proximal medial arch and paresthesia along the lateral and medial plantar nerves.” Paresthesia is the pins-and-needles prickling sensation that occurs due to nerve entrapment or restriction. TTS is a painful and debilitating condition of the foot that results from compression of the posterior tibial nerve. It is similar to the well-known carpal tunnel syndrome that is seen in the wrist.
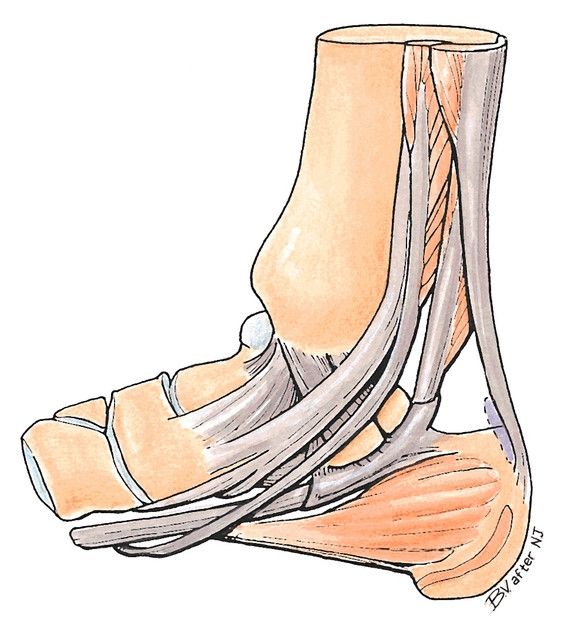
The tibial nerve enters into the foot behind the medial malleolus and under the fibrous flexor retinaculum. The flexor retinaculum ligament is the dense band of fascia that runs from the medial malleolus to the calcaneus, covering and protecting several flexor tendons, blood vessels, and nerves. The tarsal tunnel (TT) is the narrow space between the flexor retinaculum and the medial talus-calcaneus.
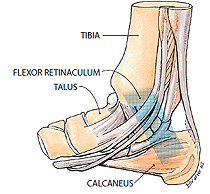 |
| Figure 1. Tarsal tunnel, medial right foot. |
It is believed that Tarsal Tunnel Syndrome occurs when there is traction on the tibial nerve and compression by the flexor retinaculum. It is frequently associated with moderate to severe pes planus indicating a strong biomechanical component to both the etiology and the treatment. Anything that takes up space in the tunnel can increase the pressure, so TTS may also arise from swelling in the tissues, arthritis, or tumors. In addition, the symptoms can be constant or intermittent.
Tarsal Tunnel Syndrome usually causes a vague pain in the sole of the foot, and patients will describe it as a “burning or tingling” sensation. It is seen among athletes and active people who stress the medial ankle area and make the tendon prone to swelling, especially if they are standing or walking for long periods. It may also occur as the result of a sprain or other traumatic injury. Frequently, the pain increases with activity and worsens as the day progresses. The symptoms may be reduced with rest. Diagnosis can be made using an electromyogram nerve-conduction test, which measures sensory and motor responses and how fast nerve impulses travel along the nerve. If the test shows that impulses are travelling slowly across the ankle, it may confirm restriction of the tibial nerve in the channel. Other tests include Tinel’s Sign, which is a shooting tingling sensation in the distal limb that occurs when the skin is tapped with a finger at the level of the irritation.
The Biomechanics of Tarsal Tunnel Syndrome
There is a quick and simple test that helps diagnose Tarsal Tunnel Syndrome. Hold the foot in maximal dorsiflexion and eversion for 10-15 seconds with the MPJs dorsiflexed. This creates non-weight-bearing subtalar joint (STJ) pronation and tenses the flexor retinaculum. If local tenderness occurs or there is tingling on the plantar aspect of the foot, there is a strong likelihood of TTS. The corollary of this test indicates that maintaining the foot in a less everted, more neutral position will alleviate symptoms.
Cadaveric studies have also determined that there is an increase of pressure in the TT compartment when the foot is pronated as compared to the neutral position. It was also noted that there was less pressure in the channel when the foot was slightly plantarflexed and inverted. (Author’s note: For a full set of references on the biomechanics of TTS, see “Rethinking Tarsal Tunnel Syndrome,” by Paul R. Scherer, DPM, Podiatry Today, December 1, 2004.)
There are several proposed causes of TTS, but frequently a specific etiology cannot be identified.
Anatomy: The flexor retinaculum blends with the plantar fascia, and both are anchored at the calcaneus. It has been proposed that tension on the plantar fascia—due to pronation—stretches the flexor retinaculum, decreasing the channel size and restricting the tibial nerve. Thus, a valgus heel and a pronated foot may well contribute to the condition.
Trauma: Compression on the nerve may be caused by traumas, sprains, contusions, ankle fractures, or post-surgical complications, including swelling.
Tumors and Inflammation: Swollen varicose veins, soft tissue tumors, edema secondary to diabetes, rheumatoid arthritis, and many other conditions can cause swelling that disrupts the tibial nerve in the TT.
The cause of TTS helps determine the best treatment. Rest, nonsteroidal anti-inflammatory drugs, and direct cortisone injections may be prescribed to control the symptoms. Physical therapy is also quite helpful in reducing symptoms. Stretching exercises to improve flexibility in the calf muscles will encourage the tibial nerve to glide within the TT. Other modalities such as heat, ice, ultrasound, and electrical stimulation are also useful.
Managing Tarsal Tunnel Syndrome
Custom foot orthotics are an excellent way to control rearfoot motion and maintain the calcaneus in a more vertical position. Typical prescriptions will include a deep heel cup (>15mm) and some degree of extrinsic rearfoot posting. The orthotic material should be semi-rigid—providing stability—and the cast modifications may include a medial heel skive to increase the ground-reaction force. If the patient will tolerate it, a medial flange will further support the longitudinal arch. Finally, a heel lift of 1/8 in.-1/4 in. will slightly plantarflex the foot and reduce pressure in the TT.
The effectiveness of orthotics depends on the type of footwear that the patient will use. First, ensure the patient wears well-fitting shoes with removable inlays that will accommodate the device. Second, the shoe itself can provide a component of support. Strong, high counters and firm outsoles will buttress the orthotic and resist the tendency of the ankle to collapse. External shoe modifications such as a medial flare may also provide some benefit.
In more advanced cases, when the syndrome is of a mechanical origin, a plastic-in-leather ankle gauntlet, AFO, or other brace may be prescribed. Again shoe fit will be a concern, but all of these devices will further restrict STJ and rearfoot motion, alleviating the pain.
If all of the conservative options fail to relieve the symptoms, surgery may be a last resort. Doctors are slow to consider this option because there is a high incidence of post-surgical complication. The procedure involves cutting the flexor retinaculum along the course of the nerve. This releases the tibial nerve, which creates more space in the TT. Post-surgical care involves temporary casting, walking with crutches, and a gradual return to activity including exercises to stretch and strengthen the muscles of the lower limb.