When treating partial foot amputees, practitioners are faced with several issues. First and foremost is limb preservation. This is achieved by limiting the destructive forces of pressure, shear, and friction. Second is the restoration of gait function, which attempts to manage the changes in biomechanics, center of gravity (COG), limb length, and propulsion. These goals should not be viewed as competing. The more that gait function is restored, the easier it is to preserve the foot. When managed properly, it is possible to restore much of the foot function and return it to its role as a stable, dynamic, propulsive lever arm.
Limb Preservation
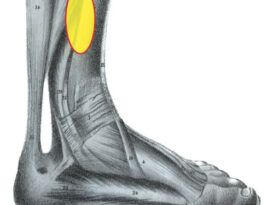
Many of the partial foot amputations that we treat are secondary to progressive disease processes, the most common of which include diabetes and Charcot joint disease. Advanced neuropathy leaves the foot insensate. This can escalate to a point where the patient, not feeling pain or any destructive forces acting on the residual foot, will unwittingly generate soft tissue damage that may eventually lead to ulcerations. In addition, the loss of sensation and proprioception leave some patients feeling clumsy and awkward, which often results in an altered gait. Thus, the remaining portion of the foot is often considered “at-risk,” and frequently further breakdown occurs within a year or two. To preserve the foot, we must manage this damaging triad of pressure, shear, and friction.
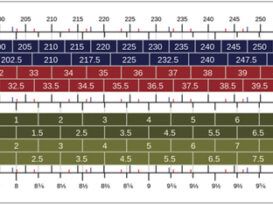
In physics, pressure is calculated by determining the force acting over a given surface area. If a partial foot amputee’s weight remains constant, there will be an automatic increase in pressure on the foot with less surface area. Persistent elevated pressure can lead to loss of tissue viability and the onset of a wound. These forces can be dispersed using an orthotic with a socket-type design, distributing pressure over a greater area. Soft interfaces also help reduce peak pressures.
Shear forces are external forces that act parallel to a plane. In terms of the foot, we can understand this as the tension and stretching of the skin that occurs when there is movement against a surface. Anatomical shearing is also created by bone moving on the inside of the skin, creating soft tissue breakdown from the inside out.
One definition of friction is the rubbing of one body or surface against another. Improper orthotic design or ill-fitting shoes can create an environment where excessive friction occurs, leading to blisters and skin breakdown. Friction may lead to skin callus formation, which can be a precursor to ulceration. Smoother surface materials such as Plastazote will be less likely to generate friction compared to rougher, more gripping top covers. Sometimes the post-surgical foot presents other complicating factors if it is not balanced correctly or if there are any boney prominences or skin anomalies.
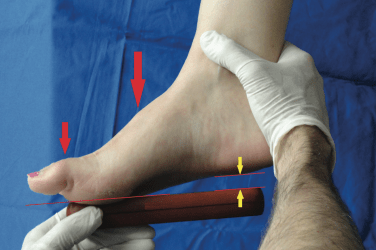
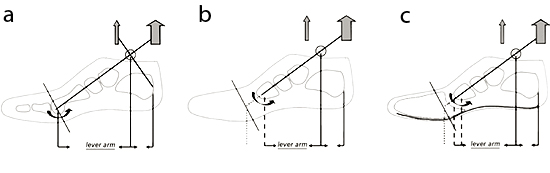 Figure 1
Figure 1
Pressure and shear occur in an amputated foot because of its smaller surface area and the inherent imbalances that are created when distal portions of the foot are removed. Consider a normal foot in the sagittal plane hinging at the ankle (Figure 1a). The relatively long lever arm of the midfoot-forefoot is balanced by the large gastroc-soleus complex. After any significant amputation, the shortened anterior lever arm will be overpowered by the strength of the posterior muscle group (Figure 1b). Muscle contraction will create increased pressure and shear at the distal end of the remaining foot. One objective, then, becomes to restore the functional length of this lever arm to absorb force and protect the remaining foot (Figure 1c).
Gait Restoration
Studies have shown that walking and exercise help patients with diabetes control their weight and blood-sugar levels, in addition to myriad other health benefits and a better quality of life. Recreating a normal, fluid, and symmetrical gait are important considerations in the rehabilitation of partial foot amputees.
 Figure 2
Figure 2
A consequence of partial foot amputation is the emergence of an unintended leg length discrepancy (LLD). A transmet, Lisfranc, or Chopart amputation removes critical anchoring tendons and muscles from the foot; this results in arch collapse and a rearward migration of the calcaneus. The net effect of this ankle plantarflexion is a lower calcaneal angle that introduces a LLD (Figures 2 a-c). In addition, regular shoes become harder to fit as the calcaneus moves posteriorally.
It is proposed that a socket-type foot orthotic for the amputee could address both the loss of anatomical position and the functional LLD by building up the shell with an appropriate anterior wedge and posting. This would dorsiflex the residual foot to some degree, restoring anatomical position and providing a lift to rebalance the malleoli.
Another factor influencing amputee gait is COG. Seeking stability, the patient will often shift toward the uninvolved side. If limb length and biomechanical function can be restored on the involved side, there will be a more normal transfer of COG, thus minimizing trunk sway during ambulation.
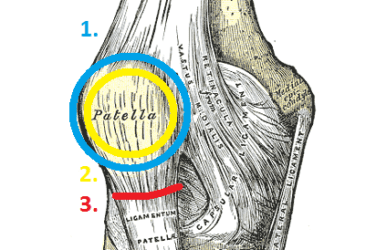
Finally, any amputation of the hallux reduces or removes the function of the windlass mechanism, which is one of the stabilizing factors in the moving foot. The medial aspect of the plantar fascia winds under the first metatarsal phalangeal joint (MPJ), and it is pulled taut when the hallux is dorsiflexed during toe off. The effect is to pull the bones of the foot into a close-packed position and convert the arch into a rigid propulsion lever. Loss of this mechanism leaves the bones of the foot “loose” during critical third rocker.
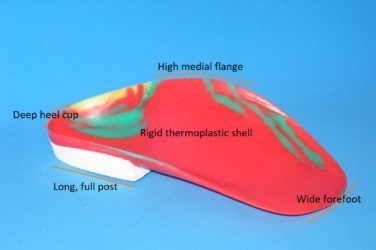
Orthotic Design
Traditionally, many orthotic designs have been used for partial foot amputees including filler prostheses, sole stiffeners, immobilizing AFOs, and combinations of these-but sometimes function is sacrificed for protection. Rocker soles are commonly used to aid toe off and help progression, especially when the shoe incorporates a stiffener. Our primary goal is to create a device that will protect the residual foot while also allowing gait restoration.
A number of pre-fabricated, carbon-fiber AFOs are available that could work to restore the lost lever arm function. They use various combinations of medial and lateral struts with either anterior or posterior shells. In principle, a lateral strut is generally preferred to a medial strut. During normal function, the foot pronates at initial contact, and that natural motion would be away from a lateral strut.
An anterior shell is also preferred to a posterior shell. Most of the shearing forces will occur during gait in the third rocker. The strut allows an energy transfer and transmits those forces to the anterior shell. If the anterior shell comes to tibial tubercle height, it will optimize the device’s lever arm function and distribute those forces over as wide an area as possible. The foot plate can be engineered to initially direct the forces of ambulation toward the shoe break.
Correct positioning of the foot orthotic is critical for optimizing function and patient comfort. The anterior shell of the AFO is aligned to the tibia and then the socket is placed on the foot plate to maintain that alignment, ensuring even pressure distribution along the shell. A soft interface must be added to the interior aspect of the anterior shell to ensure there is no skin breakdown along the tibial crest.
Proposed Solution
As a working hypothesis, we propose a socket-type orthotic with anterior wedging, lifts, and posting on a full foot plate dynamic carbon AFO. The socket-type orthotic will disperse pressure; anterior wedging dorsiflexes the foot, thereby realigning the calcaneal angle; lifts and posting address any LLD; when used with a full foot plate dynamic carbon AFO, this will provide the necessary combination for limb preservation and gait restoration (Figure 3).
 Figure 3
Figure 3
A full foot plate dynamic carbon AFO will restore the lever arm to counteract the plantarflexion moment from the posterior muscle group. Ideally, a carbon-fiber foot plate that is more stable at the midfoot with the dynamics tapering (thinning) down toward the toe will direct the forces toward the shoe break. Some of that force can be transferred via a strut to the anterior tibia and can then be reflected back during the propulsive gait phase. The AFO will also act as a transferable sole stiffener.
This concept has shown great potential in limited trials. We are hoping that practitioners will be interested in getting involved in a larger trial using a straightforward and simple before-and-after assessment so that we can test this modality and present the results more scientifically. If you are interested in reading a fuller presentation of these ideas, learning the casting method, or participating in the trial, please e-mail the lab.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York, New York. He can be reached at seamus@hersco.com or by visiting www.hersco.com.
Robert Meier, CO, BOCO has more than 30 years of experience in orthotics, with a specialty in closed-chain functional gait biomechanics.