Adult-Acquired Flatfoot (AAF) is the term used to describe the progressive deformity of the foot and ankle that, in its later stages, results in badly deformed and collapsed feet. It has been written about since the 1980’s and is most readily associated with posterior tibial tendonitis. AAF is caused by a loss of the dynamic and static support structures of the medial longitudinal arch (MLA) resulting in an incrementally worsening plano-valgus deformity.
Over the past 35 years researchers have attempted to understand and explain the gradual but significant deterioration that can occur in foot structure that ultimately leads to painful and debilitating conditions. What begins as a predisposition to flat foot can progress to a collapsed arch, then the more severe posterior tibial tendon dysfunction (PTTD) and ultimately a fixed deformity with significant calcaneal valgus, ankle pain and forefoot abduction. Left untreated the PT tendon can rupture and the patient may require an AFO or an arthrodesis fixation surgery to stabilize the foot in order that they remain capable of pain-free walking.
Foot Mechanics
The symptom most often associated with AAF is PTTD but this is only one step along a broader continuum. The PT muscle is an important dynamic stabilizer of the medial longitudinal arch that works simultaneously in the frontal and transverse planes. When the muscle contracts and acts concentrically it both inverts and adducts the foot. When stretched under tension, acting eccentrically, its function can be seen as a pronation retarder. The integrity of the PT tendon and muscle is crucial to the proper function of the foot, but it is far from the lone actor in maintaining the arch. There is a vital co-dependence on a host of other muscles and ligaments that, when disrupted, leads to an almost predictable loss in foot architecture and subsequent pathology.
The structural soundness of the foot depends on the alignment of its bony facets, which in turn relies heavily on the integrity of the ligaments and tendons. The smooth operation of the Windlass mechanism, another dynamic stabilizer, pulls the plantar fascia taut and stiffens the foot naturally when heel lift begins. If the structure is less stable excessive force is placed on the muscles, tendons and ligaments. For example, if the foot remains in pronation and fails to re-supinate at the critical point of heel lift, body weight acts as a deforming force on its unlocked joints. A clinical indication of this is prolonged pronation of the Sub-Talar Joint, seen as extended calcaneal valgus late in the gait cycle.
Beneath the foot the PT tendon travels from medial to lateral in an anterior direction and the peroneal tendons cross lateral to medial. The long and short plantar ligaments and the Spring ligament connect the bones of the tarsus. If the foot does not stiffen for propulsion each of these ligaments can begin to attenuate leading to deterioration and a loss in foot shape. In one study1 in order to accomplish the collapse of the hindfoot and midfoot that is typically seen in Stages II and III PTTD deformities researchers had to sever multiple ligaments including the Spring ligament, the plantar aponeurosis, and the Deltoid ligament. This demonstrated the severity of AAF goes far beyond a strain on the PT tendon alone, and it affects all of the dynamic and static stabilizers of the foot.
Risk Factors and Stages
Risk factors for developing AAF include a predisposition of flatfoot, high body mass index and being female. A typical presentation is a sedentary, middle-aged to elderly woman with pain and swelling along the medial ankle of one leg. Diabetes and hypertension are associated co-morbidities. The progression of AAF was originally classified into distinct stages by Johnson and Strom2 in 1989 (Table 1). Subsequently the stages and associated treatment protocols have been refined, and Stage II is subdivided into 5 categories A – E. In fact, there are now several different classification systems for AAF. Debate remains as to the process of development of PTTD: whether the ligaments attenuate first, putting strain on the tendon, or strength deficits jeopardize the ligaments.
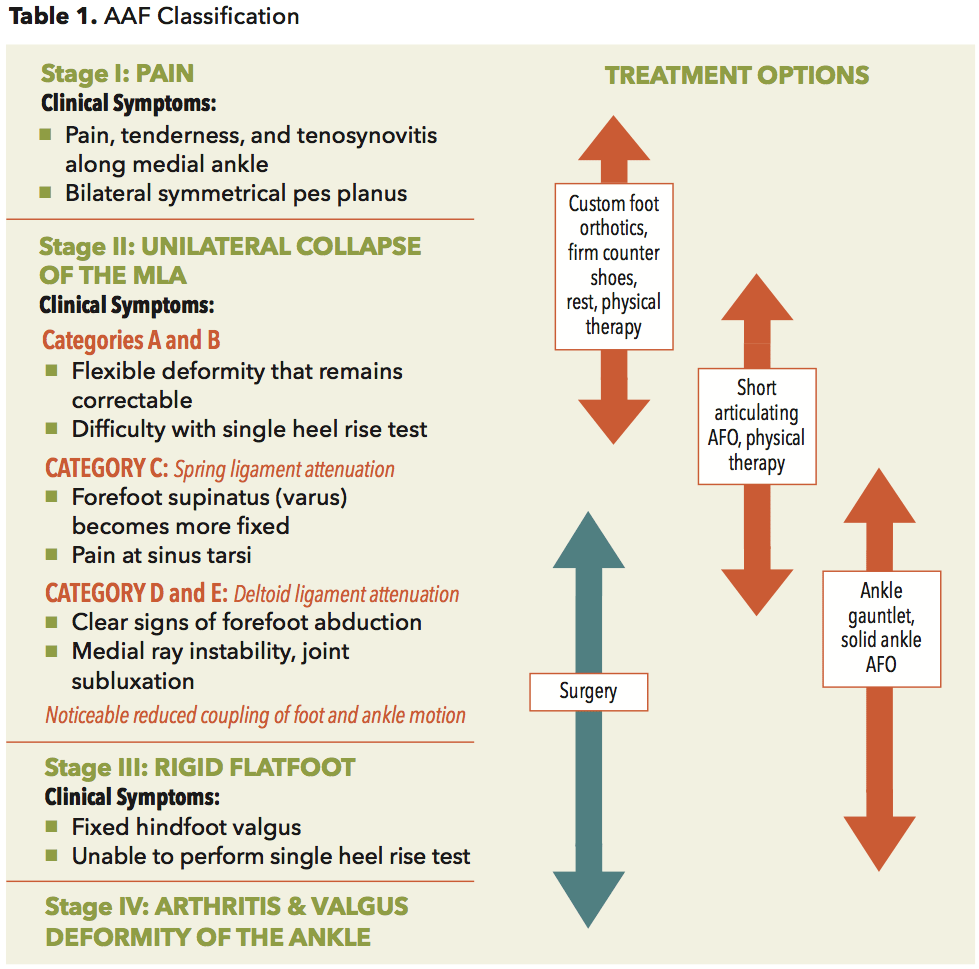
(Developed from the Johnson and Strom PTTD classification).
Progression
Studies show there is a notable increase in gliding resistance in the PT tendon of patients with flatfeet. The path of the PT tendon, much like a pulley, takes a sharp 90 degree turn around the distal end of the medial malleolus which increases the force required to invert the foot. It is speculated, if the tendon weakens with repetitive stress at this friction point and the supporting ligaments of the medial ankle are constantly strained over time they will deteriorate. What presents as a tenosynovitis in Stage I develops into a more painful asymmetrical flatfoot deformity in Stage II. Attenuation of the Spring ligament marks a significant step as it spans the talonavicular and subtalar joints. This creates the noticeable MLA collapse and forefoot abduction as the head of the talus becomes more prominent medially. Patients will have difficulty performing the single heel rise test. By Stage III the triangular Deltoid ligament, a primary stabilizer of the talocrural joint, has also been severely compromised and there is significant ankle subluxation. In the later stages there is usually a talar tilt, ankle arthritis and a fixed abduction of the forefoot.
Besides losing foot and ankle structure the mechanical coupling between the foot and lower leg is also compromised. In a normal foot there is a synergy in motion where internal tibial rotation contributes to pronation, and external tibial rotation induces supination. Comparing the network of ligaments around the ankle to rubber bands, when the bands are taut motion transfers easily between the two. However, given the flaccid bands associated with advancing AAF the foot becomes less directly connected to the lower leg, and motion is loosely coupled between them.
This development informs the choice of bracing as AFO’s can augment the relationship between the two.
Treatment Options
Appropriate treatment for AAF considers the patient’s current symptoms and attempts to reduce the pain and restrict further damage to the foot while allowing ambulation. In the early stages orthotic and pedorthic solutions can address the loss of integrity of the foot’s support structures potentially retarding further destruction. As a general principle, orthotic devices should only block or limit painful or destructive motion, without reducing or restricting normal motion or muscle function. Consequently the treatment must match the stage of the deformity.
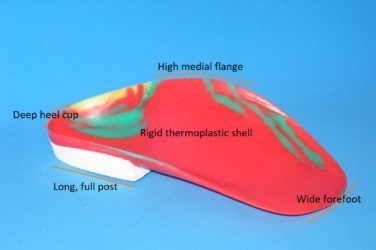
In Stage I the patient can be prescribed custom foot orthotics and well-fitting supportive shoes. The goal is to support the foot and, if possible, minimise the effects of late stage pronation. Orthotic modifications such as deep heel cups, medial heel skives, medial flanges and rearfoot varus posts can all help redirect and alter ground reaction forces. In some cases requesting a 1st ray cut-out or Kinetic wedge can restore lost motion at the 1st MPJ which may enhance the stabilizing effect of the Windlass mechanism. Hiking boots with stiff high counters reinforce the medial column and provide support above and below the ankle. Icing and anti-inflammatory medications can also be prescribed. In the early stages physical therapy has proven to be quite effective. Targeted programs stretching and strengthening the muscles of the foot and ankle have shown to be very beneficial.
As Stage II further develops foot orthotics may no longer offer sufficient support to control the foot and ankle complex. As key ligaments in the foot attenuate and eventually rupture the important tibial coupling effect is lost. Foot motion becomes increasingly disconnected from tibial rotation. It becomes necessary to graduate to an AFO that will control the foot and compensate for the loss of motion across the ankle joint.
Short articulating AFO’s such as the Richie Brace are well suited to Stage II treatment. The custom foot orthotic, deep heel cup and high medial and lateral struts enhance the tibial coupling. Patients tend to accept these devices as they can often be worn in sneakers or extra depth shoes. More importantly, using articulating ankle joints enables full range of motion in the sagittal plane, allowing patients to walk relatively normally. Hinged devices appear advantageous as they still recruit regular muscle activity which helps hindfoot inversion and controls forefoot abduction(3). In cases where the hindfoot is still correctable, and the tendon is not overly sensitive, a Sustentaculcum Tali (ST) cast modification may be incorporated into the design to provide improve rearfoot control.
In late Stage II and Stage III it becomes necessary to provide more control. If the midfoot becomes destabilized and forefoot lateral splay continues, plastic-in-leather ankle gauntlets such as the Arizona type can be employed. Interestingly, medial flanges are no longer recommended at this stage as they may actually contribute to forefoot abduction. One study demonstrated that an ankle gauntlet with a lateral extension reduced forefoot abduction in Stage II patients(4). Extending the thermoplastic trimline to just behind the 5th met head appeared to maintain correction of the MLA, and increase hindfoot inversion.
Gauntlets made from rigid polypropylene are much more restrictive and may require a change of footwear to a wider lasted shoe with an open throat. Chukka style shoes or high tops are recommended as they provide more support and help keep the AFO properly seated. A rocker sole can be added to the shoe to replace some of the lost motion at the ankle. There are also several surgeries that can be performed to selectively stabilize the major joints in the foot and improve the biomechanics and foot function. In more advanced cases, when the patient is heavy or perhaps not a good surgical candidate, it may be necessary to consider a solid ankle AFO or even a traditional double metal upright style brace.
Conclusion
In its simplest form AAF is recognized as the painful incremental deterioration of the support structures of the normal foot. PTTD is just one step on a longer journey that typically begins with a pre-existing flatfoot. Late-stage pronation increases the loads acting on the dynamic and static stabilizers of the medial foot and ankle, undue strain is placed on critical ligaments and joints are compromised. Gradually proper structure in the foot is lost. Appropriate treatment depends on the level of disruption to foot function. Orthotics and AFO’s support and retard the progress of AAF, especially in Stages I and II. In the worst cases reconstructive surgeries or complete ankle immobilization may be necessary.
Author’s note: For a more complete review of the etiology and staging of AAF and further references see “Biomechanics and Orthotic Treatment of the Adult Acquired Flatfoot” Douglas Richie Jr, DPM FACFAS, Clinics in Podiatric Medicine & Surgery, 37 (2020) 71 -89.
The author gratefully acknowledges the help and contribution of Dr. Douglas Richie in preparing this article.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A), is president and co-owner of Hersco Ortho Labs, New York. He can be contacted at seamus@hersco.com or by visiting www.hersco.com.
References
- Foot Ankle. 1992 Jul-Aug;13(6):327-32.
Adult acquired flatfoot deformity at the talonavicular joint: reconstruction of the spring ligament in an in vitro model.
Deland JT, Arnoczky SP, Thompson FM. - Clinical Orthopedics and Related Research. 1989 Feb;(239):196-206.
Tibialis posterior tendon dysfunction.
Johnson KA, Strom DE. - Foot Ankle Int. 2012 May;33(5):406-14.
Effect of ankle-foot orthotic devices on foot kinematics in Stage II posterior tibial tendon dysfunction
Neville C, Lemley FR - Orthopedic Sports Physical Therapy. 2016; 46(1):26-33.
An ankle-foot orthosis with a lateral extension reduces forefoot abduction in subjects with stage II posterior tibial tendon dysfunction.
Neville C, Bucklin M, Ordway N, et al.