Equinus is a common foot and ankle condition that, depending on the clinical definition, is thought to be present in the majority of the population. It is also recognized as a leading contributor to foot pathology. In simple terms, equinus is the inability of the ankle joint to dorsiflex sufficiently to allow the body’s center of mass to pass over the plantigrade foot. Any restriction in motion at the ankle joint, as the tibia moves over the foot in midstance, will produce a compensation. As this forced compensation occurs dynamically during full weight bearing, the long-term effects can be detrimental.
Equinus is believed to be a contributing cause to a wide range of diagnoses including plantar fasciitis/heel pain syndrome, Achilles tendinopathy, calcaneal apophysitis, pes planovalgus, adult acquired flatfoot/posterior tibial tendon dysfunction (PTTD) syndrome, and forefoot pathologies such as metatarsalgia, bunions, sesamoiditis, and hallux limitus. It is also strongly linked to the breakdown and ulceration of the forefoot in patients with diabetes and advanced neuropathy and the destructive effects associated with Charcot neuroarthrapathy.
Testing and Defining Equinus
The Silfverskiold test is the clinical standard for equinus. The practitioner begins by fully extending the knee. With the subtalar joint (STJ) in neutral, supinate the forefoot, dorsiflex the foot, and measure the angle of dorsiflexion at the ankle. Next, flex the knee to 90 degrees and repeat the measurement.
If there is less dorsiflexion when the knee is extended, this indicates a gastroc equinus, which is pulled tighter when the leg is straight. If dorsiflexion is equally limited with the knee flexed and extended, this points to either a soleal equinus or an osseous block. To distinguish the type of equinus, the practitioner must feel for the end range. A soft or spongy end range indicates a muscular contracture. A hard or abrupt end range occurs when there is a boney block, which can also be confirmed by x-ray.
There is no universal standard as to what constitutes equinus but rather a range indicating normal and limited motion. It would appear from several studies the most widely accepted value for static measurement of dorsiflexion at the ankle joint is 10 degrees. In a paper by DiGiovanni et al., patients with less maximum ankle dorsiflexion due to gastroc tightness had approximately twice the number of forefoot and midfoot symptoms.1 Regardless of the discrete value, any restriction of motion at the ankle that inhibits the upper body from passing over the foot will result in a forced compensation.
Anatomy
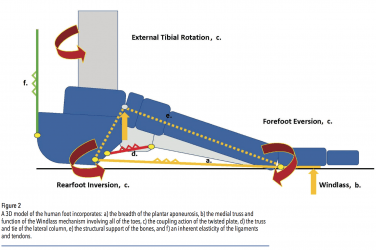
By surveying the anatomy it is possible to understand how equinus may be considered the root cause for such an array of foot pathologies. The triceps surae, consisting of the gastrocnemius and soleus, is responsible for ankle plantarflexion. The gastrocnemius originates at the condyles of the femur, crosses the knee joint, and inserts into the posterior calcaneus below the ankle joint. As a result, the gastroc affects both knee and ankle flexion. Other upper leg and thigh muscles also cross the knee joint. The soleus originates below the knee but it also inserts, via the Achilles tendon, into the calcaneus below the ankle joint. In the foot, the plantar fascia originates on the inferior calcaneus. Tracing this series of origins and insertions, it is apparent that any restriction or tightness at one link or joint in the chain may produce strain at another (Figure 1).
 Figure 1: The foot and leg seen as an inter-linked series of joints and members. In this simplified model, a restriction at one location directly affects motion at another.
Figure 1: The foot and leg seen as an inter-linked series of joints and members. In this simplified model, a restriction at one location directly affects motion at another.
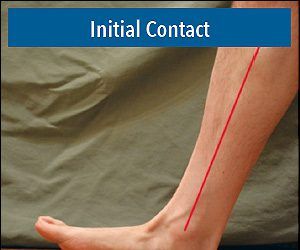
 Figure 2: Any restriction in the motion of the tibia as the center of body mass moves over the foot will require a compensation. If the STJ pronates, unlocking the MTJ, there will be potentially destructive forces acting on the midfoot.
Figure 2: Any restriction in the motion of the tibia as the center of body mass moves over the foot will require a compensation. If the STJ pronates, unlocking the MTJ, there will be potentially destructive forces acting on the midfoot.
It is often said that a chain is only as strong as its weakest link. In biomechanics, when the lower limb is subjected to the repetitive loading of weight bearing ambulation, stress will find a locus at the most restricted point in that chain or sequence—where there is the least adaptation to the required motion. In an attempt to conform with gravity and keep the weight bearing foot in full contact with the supporting surface, the body can adopt several mechanisms. These may be complete, partial, or incomplete. These compensations are the source of the harmful strain associated with equinus.
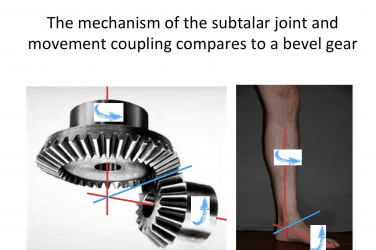
Midtarsal Joint Compensation
In midstance, if the foot is not plantigrade, the initial compensation will be from the subtalar joint (STJ). The STJ attempts to pronate the foot down to the ground. This works well when there is a frontal plane imbalance such as forefoot varus. However, equinus is a sagittal plane deformity, and the STJ has very limited motion in the sagittal plane. The foot then relies on motion at the midtarsal joint (MTJ) with potentially severe consequences. The MTJ consists of the talonavicular and calcaneocuboid joints, and it stabilizes the midfoot and forefoot. Traditionally the MTJ is considered to move along two axes: the longitudinal axis of the foot, and an oblique axis that traverses the foot. The position of the STJ is critical to the MTJ. If the STJ is fully pronated as a primary response to equinus, the alignment of the calcaneus and the talus essentially opens the MTJ, and it may then be seen as more of a universal joint. Once the MTJ is unlocked, the midfoot becomes considerably less stable, which causes the joints and bones of the forefoot to become more influenced by external forces and opens damaging pathways for a series of problems (Figure 2).
With the loss of integrity of the MTJ as a result of compensation for an underlying equinus, you may see any of the following:
- Forces inducing a collapse of the midfoot as the forefoot dorsiflexes on the rearfoot.
- A lowering of the medial longitudinal arch, potentially putting a strain on the plantar fascia.
- A “loosely packed” foot that allows a forward migration of the first metatarsal, which can lead to a blocking of motion at the first metatarsophalangeal joint. This creates a functional hallux limitus, which in turn alters gait.
- Over time, an unlocked MTJ contributes to the total foot collapse seen as adult acquired flatfoot that frequently presents as PTTD.
What makes the compensation at the MTJ most destructive is that it occurs so late in the gait cycle. Just at a time when the foot is accepting body weight and requires stability, the MTJ opens, unlocking the distal joints. This can prove to be disastrous. For example, it is not unusual to see a patient with an equinus and a ligamentous lax body type go into pronation after heel lift.
Other Compensations
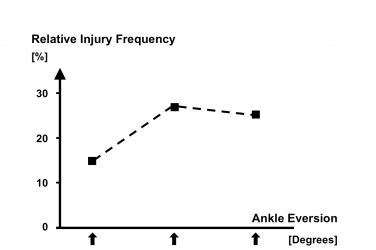
If forward motion of the tibia is restricted during ambulation, there may be an external rotation of the foot. This changes the normal line of progression from over the center of the foot to over the medial side of the foot and results in a splay gait. In cases of tight triceps, the foot may evert as the calcaneal valgus shortens the distance between the muscles’ origin and insertion. As such, many patients presenting with flat feet may be masking an underlying equinus.
Early heel rise, seen as a “bouncing gait,” is another compensation. The restricted triceps pull the heel up prematurely. A short stride, premature knee flexion, or hyperextension are other ways to reduce the required tibial dorsiflexion, yet still allows the body’s center of mass to move forward.
Uncompensated equinus occurs when the heel fails to contact the ground. A familiar albeit infrequent presentation is the equinovarus foot. This foot type usually occurs secondary to a more serious neuromuscular disease; it used to be prevalent among post-polio patients. The typical equinovarus foot has severe and fixed plantar flexion with little to no available motion at the ankle joint. These patients often have forefoot problems including heavy localized callusing and perhaps metatarsalgia. When the equinovarus is unilateral, there is an inherent leg-length discrepancy that needs to be addressed in order to keep the frame of the body in balance.
Orthoses
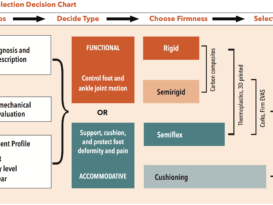
Orthotic devices can be very helpful for addressing equinus. Most simply, a heel lift that brings the ground up to the foot can negate many of the deleterious effects. However, this can also encourage a permanent shortening of the gastroc-soleus. Sometimes a variable height heel lift can be employed to provide immediate relief. This works best with a comprehensive program of physical therapy and stretching. Then the lift height can be reduced over time as the posterior muscle group lengthens. Orthotics can also incorporate a heel lift. More importantly, foot orthotics can support the midfoot and provide control of the arch. By influencing the timing, extent, and duration of pronation, custom foot orthotics will limit the most destructive effects of an inappropriately unlocked MTJ. Finally, patients need to wear well-constructed and properly lasted shoes. Shoes with firm counters and a reasonable heel pitch (>12mm) provide the best combination of support and plantarflexion to reduce the worst effects of equinus.
In worse cases, it may be necessary to use a solid ankle AFO. This works by restricting ankle joint motion, directly linking the foot and lower leg and thereby reducing the destructive tendencies. If conservative treatments fail, surgical techniques are also available to address the issue. Physicians may choose to do a tendo-Achilles lengthening or a gastroc recession to restore range of motion to the ankle. In summary, equinus is a highly prevalent and potentially destructive condition with severe long-term consequences to foot health. It should become a standard part of every patient evaluation to test for and address any restriction in ankle joint dorsiflexion.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York, New York. He can be contacted at seamus@hersco.com or by visiting hersco.com.
Reference
- DiGiovanni, C. W, R. Kuo, N. Tejwani, R. Price, S.T. Hansen Jr., J. Cziernecki, B.J. Sangeorzan, Isolated gastrocnemius tightness. The Journal of Bone & Joint Surgery. 2002; 84-A(6):962-70.