When I first started in this field well over 12 years ago I found myself in the unenviable position of running a company that had outdated products. The entrepreneurial zeal that my brother and I shared allowed us to become owners of an “arch support” business with a lot of historyand a seemingly short future. It was time to sink or swim, so I attacked the textbooks and journals to learn as much as possible about the current thinking on custom orthotics, the foot and its diseases, and orthopedic shoes. That same year I also became a certified pedorthist. Over the next few years the material that I read left me a little confused. There were plenty of discussions and articles written on foot orthotics and the anecdotal evidence of their efficacy. However, there was certainly no consensus on a complete theory of the biomechanics of the foot.
Leonardo da Vinci said, “The human foot is a masterpiece of engineering and a work of art.” Each foot comprises 26 bones, 19 muscles, and 107 ligaments. Great work has been done to develop an understanding and standards of practice regarding the foot and its function, but it is hardly surprising that the foots workings cannot be captured in one or two statements or even a single, compact theory.
History |
| Care for the foot and its diseases dates back centuries. The history of external foot care began with shoemakers. Historically the foot was described by external appearance. Observable differences such as arch height (low or high), mobility (rigid or flexible), or obvious deformities (bunions, calluses, hammertoes, etc.) were the basis for categorizing the foot and developing treatment protocols. Physicians were very much treating the symptoms without understanding the underlying causes.
Before World War II surgical procedures were not as advanced, so orthopedic doctors often turned to the shoe and arch support industry for mechanical or functional solutions to foot and ankle problems. The first employees in the arch industry were mainly Eastern European craftsmen who brought their expert knowledge of shoe making and orthopedics to America. People with leg length discrepancies, post-polio syndrome, clubfoot, or just chronically flat feet all benefited from internal and external shoe modifications. Lifts, metatarsal supports, wedges, depressions, cushions, etc., could all be added to an arch support to give lasting relief. Shoemakers and shoe repair specialists could order prefabricated leather shells and components and then adapt and fit them for a particular patient. Orthopedic companies made a variety of custom and prefabricated foot products from materials such as sole leather, cork, rubber, and even stainless steel. These materials could be formed to provide high medial flanges and firm support for the midfoot, but deep heel cups were not possible. Despite the limitations of materials and understanding, the arch support industry did develop “results-based” knowledge that provided welcome relief to generations of patients. |
With the continued development of modern medicine in the mid-20th century, the podiatric colleges began to focus in earnest on the biomechanics of the foot. Could a “normal” foot be described accurately, and could this description lead to an understanding of foot pathology? The late Merton Root, DPM, is the name most often associated with the initiative to bring science to the internal workings of the foot. Root was a researcher at the then California College of Chiropody in San Francisco, and he developed a theory that now bears his name. The initial work of the researchers was to try and describe “normal mechanics” and normal joint motion, and from there deduce how abnormal function produces deformities.
Root Theory of Foot Biomechanics
Although rather involved, the Root theory of biomechanics rests on three key concepts.
- It became clear that there was a critical mechanical relationship between the subtalar joint (STJ) and the midtarsal joint, and that this relationship could be the origin of mechanical foot dysfunction. Understanding this would allow
- professionals to treat the real cause of foot problems, not just the symptoms.
- By developing a “criteria defining a normal foot” Root realized that “for every degree of motion of the STJ the plantar contour of the heel changed slightly.” Thus, changing the plantar contour of the foot would change the position of the STJ. This was a vital cause-and-effect: if you can alter the STJ using orthotics, then you also affect the motion of the midtarsal joint.
- Casting feet in a non-weight-bearing “STJ-neutral” position was a method of standardizing and comparing one foot to another. This was a consistent yardstick that could be employed across practitioners, allowing measurement of the rearfoot-to-forefoot relationship.
|
|
The development of these ideas through untiring trial-and-error led to many conclusions including that certain foot types had predictable and describable foot dysfunction.
Pathological Foot Types
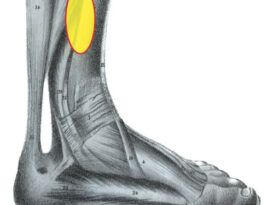
- With the heel in the neutral position (calcaneus vertical) some feet will display forefoot varus (medial forefoot off the ground), which will lead to compensatory eversion (pronation at the STJ). See figure 1.
- With the heel in the neutral position (calcaneus vertical) some feet will display forefoot valgus (lateral forefoot off the ground), which will lead to compensatory inversion (supination at the midtarsal joint). See figure 2.
- A foot with an inverted calcaneus (relative to the lower leg) in the neutral position has a rearfoot varus.
In each case the orthotic needs to support the plantar heel and be “bent” in such a way as to support the forefoot in relation to the rearfoot if it is to prevent abnormal STJ or midtarsal joint position or motion. In effect, the angular difference between rearfoot and forefoot will translate as a twisting across these joints unless the orthotic intervenes.
Roots theory was a major step forward that brought a scientific understanding to the internal workings of the foot. The research also coincided with the emergence of new materials for the orthotic industry. Thermoformable plastics, acrylics, and urethanes in various thicknesses and durometers could all be pulled over corrected plaster feet, allowing far greater accuracy and diversity in orthotic design. In addition, deep heel cups to help control rearfoot motion and position were now possible.
Further enhancements to Root’s work have occurred over the years. One popular cast modification is the “Kirby heel skive.” Named for Kevin Kirby, DPM, it involves shaving some plaster from the medial heel to increase ground reactive forces under the medial side of the STJ axis.
Although not a complete description of the mechanics of the foot and lower extremity, Roots work serves as a good starting point. Many objections have also been raised to the Root theory:
- Is the STJ neutral position the optimum reference point for “normal” foot function?
- If the foot is only in STJ neutral for a fraction of the gait cycleduring heel contactwhy should the cast and the orthotic be built around this single position?
- Is the STJ-neutral method of casting reliably accurate and repeatable across practitioners?
- Can a round heel really be expected to stand vertically inside a rounded heel cup when rotational forces are present?
- Given that the heel has significant soft tissue and a fat pad, how much control can an extrinsic wedge really provide?
Despite these objections and more, Root’s theory has proved effective in providing functional and therapeutic foot orthotics to millions. With the more recent development of computerized gait analysis, force plates, video technology, and sheer processing power, many new hypotheses in foot function have emerged. Ultimately good practitioners need to be aware of these developments, but treating actual patients still requires a true blend of technical knowledge, fine observation, and a good amount of hands-on experience.