Lateral ankle sprains are among the most common sports injuries and account for a significant percentage of time lost due to injuries. Athletes returning to activity too soon after a severe ankle sprain may be at risk for longer-term ankle instability. The foot and ankle’s functional anatomy is complicated, but understanding it is critical if treatment protocols are to be effective. The good news is research supports the use of foot orthotics to improve balance-a key component for preventing permanent ankle damage.
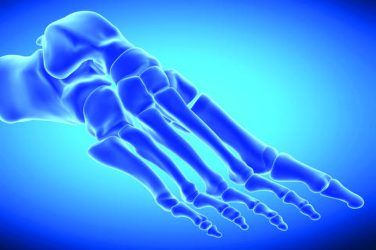
Acute ankle sprain occurs when there is a sudden twisting of the ankle leading to pain, swelling, and loss of activity. This may happen when descending stairs, walking on uneven surfaces, or being tackled in a football game. The stresses from a sudden forceful pedal inversion and the loss of balance result in damage to some of the lateral ankle ligaments. Among the lateral collateral ligaments, the anterior and posterior talofibular ligaments and the calcaneofibular ligament are most vulnerable in a sprain and may be attenuated or torn in an acute incident.
There are several systems that classify acute ankle sprain. According to the West Point Ankle Sprain Grading System and Chapman’s grading system, Grade I indicates a strain but no ligament tears, and the patient can still bear weight without assistance. Grade II represents a partial ligament tear with moderate edema, a significant limp, and reduced ability to walk without assistance. In Grade III there is a complete tear, severe edema, and no ability to bear weight. Treatment is prescribed based on the physician’s assessment and other evidence, such as x-rays. A popular mnemonic, PRICE, is often followed in the healing process.
The PRICE of Ankle Sprains
- Protected weight bearing: Initiating weight bearing soon after an injury can reduce swelling and help improve and speed healing. The ankle joint is more stable when it is dorsiflexed, whereas a non-weight bearing resting foot will naturally tend to plantarflex. In more serious cases the patient could be fitted with a CAM walker to begin immediate, protected weight bearing. Even partial touch down will compress the ankle joint and stimulate muscle action.
- Rest: While encouraging early weight bearing, it is also important to rest the foot at least until the pain and edema begin to lessen. There is a necessary balance between encouraging early mobilization and protecting the patient from pain.
- Ice: Periodically icing the ankle will help reduce swelling, improve circulation, and aid recovery.
- Compression: Wrapping the ankle assists in controlling edema, which has the advantage of enhancing ROM. It may also allow for earlier weight bearing and some pain reduction.
- Early mobilization and aggressive rehabilitation: Early intervention speeds healing and, in the long term, may reduce recurrence. This will include non-weight bearing exercises such as plantarflexion and dorsiflexion, inversion and eversion, and toe curls. Eventually balance training and restoring proprioception and postural control are the best defense against a recurrence.
Chronic ankle instability is recognized as repetitive bouts of lateral ankle instability resulting from numerous ankle sprains or an inherent weakness in the ankle structure. Unfortunately, ample evidence suggests that protocols are sometimes rushed after an acute sprain, even though ruptured ligaments need up to six months to repair. Poor initial treatment in the acute phase and other factors such as age can lead to this debilitating condition. The resulting chronic instability may be considered functional or mechanical.
Functional instability refers to neuromuscular or proprioceptive deficits diminishing control of the talocrural joint. This is the recurring chronic condition in which the ankle seems weaker and is more easily sprained. Mechanical instability describes a loss of the intrinsic stability of the ankle. This may occur from overstretched ligaments that become lax after a significant sprain. It can also indicate restricted range of motion (ROM) in the ankle or foot joints. The effects of these instabilities overlap and a combination of both is believed to be at work in recurring ankle injuries.
The Neuromuscular System
Neuromuscular control of the ankle, which affects functional stability, has four major components: proprioception, muscle strength, muscle reaction time, and postural control, which includes balance.
Proprioception is the body’s ability-independent of vision-to sense stimuli arising from within regarding position, motion, and equilibrium. In the ankle, this sense is gained primarily from afferent (sensory) nerve terminals in muscles and tendons, and mechanoreceptors in the capsule and ligaments. Feedback from the surrounding skin and tendons also provides vital information, which explains why interventions such as ankle taping or wearing high-top shoes can be beneficial for preventing injuries.
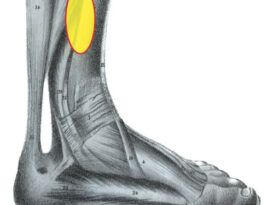
The efferent (motor) loop also plays its part. The primary evertors of the foot are the peroneal muscles; they act eccentrically against inversion. Damage to the peroneals can weaken them and delay muscle reaction time. This allows an imbalance to develop before a corrective response is initiated. As a result, physical therapy is an important aspect of any rehabilitation program to restore strength and essential muscle cues regarding position.
Postural control is the ability to maintain or restore a state of balance in any posture or activity; loss of this control is a factor in chronic ankle instability. The Romberg test, wherein the patient closes his or her eyes and stands on one foot, is used to assess postural control and determine a patient’s sense of balance. The sole of the foot plays a critical role in providing feedback on balance and sway. There are three distinct types of mechanoreceptors on the plantar surface that respond to pressure and inform the central nervous system, which then activates muscles in the lower leg. Properly designed foot orthotics can enhance these pressure sensor systems and provide clear signals to the body.
The neuromuscular system is a dynamic stabilizer of the ankle joint, but its action is complex, interdependent, and not well understood. In one study, researchers applied an anesthetic block to the critical anterior talofibular ligament and then tested for proprioception and balance.1 To their surprise, they found that balance improved. In another study, researchers provided posted prefabricated orthotics to half of the cohort and measured postural control.2 Initially they saw little difference, but after four weeks the study group showed significant improvements, indicating that there may be a neuromuscular learning phase before the full benefits of orthotics become apparent.
Biomechanics of the Foot
Another key factor in ankle stability is the mechanical operation of the foot and ankle. The talus sits at the junction of the lower leg and foot, playing a vital role in the operation of each. It has no muscular attachments and is affected by both axial rotation of the leg and frontal plane pronation or supination of the foot. This motion transfer between the leg and foot is referred to as movement coupling. In essence, when the lower leg rotates internally the foot will pronate. This is a stable position for the foot. Likewise, rotating the leg externally induces supination of the foot. Supination includes plantarflexion and inversion, which are considered less stable. Oftentimes the trigger event leading to an ankle sprain, such as landing from a jump, transmits torque from the supinated foot to the lower leg. Due to the movement coupling, sudden supination of the foot translates to rapid external rotation of the leg, damaging the lateral collateral ligaments.
The Role of Foot Orthotics
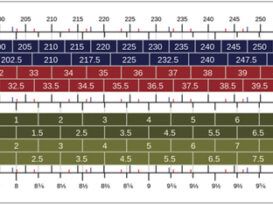
If forefoot alignment is one of the mechanical factors contributing to ankle sprain, then custom foot orthotics can be used to address the imbalance. When the weight bearing foot is inverted, pressure along the lateral border will usually be increased. Rather than just push the foot medially with a lateral wall, the use of posting under the forefoot, distal to the metatarsal heads, can rebalance forces. For example, in the case of a forefoot valgus, consider using a lateral wedge (from the fifth to the third metatarsal) extending it to the sulcus. Similarly, a plantarflexed first ray would benefit from a Reverse Morton’s-type accommodation that elevates the sulcus of the second to the fifth. In both cases you are rebalancing, attempting to evert the forefoot and bring it closer to a neutral position.

In combating chronic ankle sprains, it appears that the role of foot orthotics is to improve body position and allow greater ROM. In the past it was thought that holding the foot in a vertical position was best, and as a result, many foot orthotics were extrinsically posted to neutral. Whether the patient pronated or supinated, rearfoot posts were prescribed. With current understanding of the importance of postural control and the pressure sensors on the plantar foot, the role of orthotics has changed. The goal now is to provide ROM while engaging the sensor systems, which may allow sufficient time for the body to react when it senses sudden imbalance. This is supported by a 2012 study that provides preliminary evidence that custom foot orthotics can improve balance in older adults.3
Foot orthotics should be designed to reduce strain on the foot, improve ROM, and enhance sensory feedback. Use of an intrinsically balanced semi-rigid shell with a deep heel cup will improve plantar contact and give good mechanical support without blocking motion. Medial support and full-length cushion top covers have the advantage of activating sensors along the entire sole. Most of these orthotics should not have a rearfoot post as this restricts motion of the subtalar joint. As previously mentioned, sulcus posting can be applied to reduce internal compensations and rebalance the forefoot.
Physical therapy is an important part of rehabilitation to prevent long-term, recurring problems. Muscle strengthening, stretching, and proprioceptive and balance training will improve the overall function of the neuromuscular system, restoring balance and control. Wearing lace-up ankle braces has also shown a reduced incidence of sprains among athletes. Studies indicate there is no clear benefit to early surgery, so it is often best to aggressively treat the condition using conservative measures before choosing to undergo an operation. Ankle function and associated injury prevention is a rich topic; a 2007 review by Douglas Richie Jr., DPM, FACFAS, serves as a great reference for further study.4
References
- De Carlo, M. S., and R. W. Talbot. 1986. Evaluation of ankle joint proprioception following injection of the anterior talofibular ligament. Journal of Orthopaedic & Sports Physical Therapy 8 (2):70-6.
- Rome, K., and C. L. Brown. 2004. Randomized clinical trial into the impact of rigid foot orthoses on balance parameters in excessively pronated feet. Clinical Rehabilitation 18 (6):624-30.
- Gross, M. T, V. S. Mercer, and F. C. Lin. 2012. Effects of foot orthoses on balance in older adults. Journal of Orthopaedic & Sports Physical Therapy 42 (7): 649-57.
- Richie, D. H., Jr. 2007. Effects of foot orthoses on patients with chronic ankle instability. Journal of the American Podiatric Medical Association 97 (1):19-30.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.