Posterior tibial tendon dysfunction (PTTD) is one of the most common diagnoses of the foot and ankle, and it is more prevalent than ever due to a number of factors such as an increasingly overweight and aging population. PTTD can be seriously disabling, but there is good evidence to suggest that aggressive conservative treatment in the early stages can limit the worst effects. Medication, physical therapy, foot orthotics, ankle bracing, and shoe modifications all have a role to play in preventing the progression of the disease before surgical options have to be considered.
Anatomy
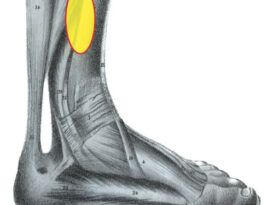
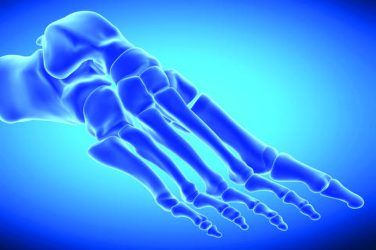
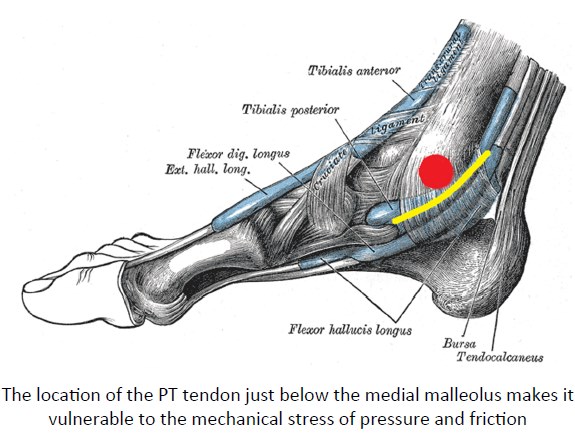
The tibialis posterior or PT muscle originates from the deep posterior compartment of the leg. The PTtendon passes posterior to the medial malleolus, slightly posterior to the ankle joint axis. It then passes medially and plantar to the subtalar joint (STJ) axis. The tendon divides into three branches and collectively these insert deep into the plantar arch of the foot, including the navicular, all three cuneiforms, the cuboid, and the bases of the first through fourth metatarsals. Due to its location, multiple insertions, and influence over several axes of the foot, the PT muscle has a critical function in weight bearing activity and plays a major role in the gait cycle. The muscle is an inverter and plantarflexor of the foot. During eccentric contraction, it is responsible for decelerating and limiting pronation of the foot following heel strike. Loss of function of the PT tendon results in a foot that is unable to stabilize the midtarsal joint, and over time the foot demonstrates increased pronation.
Because it is located immediately below the medial malleolus, the tendon is vulnerable to even slight changes in foot position. Patients with PTT insufficiency may present symptoms of pain, tenderness, or swelling along the medial ankle, a restriction of the gliding motion of the tendon, a partial tear, or a complete tear. Pathologic rupture is usually due to progressive chronic stress on an already compromised tendon, whereas a functional rupture is diagnosed when the tendon remains intact but is not functioning correctly.
Posterior Tibial Tendon Dysfunction

Starting in the 1980s, researchers began to focus on both the mechanism and effects of injuries to the PT tendon. Until that time, surgeons tended to treat the symptom by repairing the tendon, but the results were poor. Efforts were made to understand the underlying causes that led to the tendon rupture. Investigations revealed that PTTD may be considered part of a greater progressive flatfoot condition, adult acquired flatfoot (AAF), which results from the failure of multiple capsular and ligamentous structures in the foot. A more in-depth discussion of AAF can be found in “Understanding Adult-acquired Flatfoot” (The O&P EDGE, November 2014, pg. 54-7). In essence, by the time a patient presents with PT tendinosis, a series of marked changes have already occurred within the static and dynamic support structures of the foot. This has been verified through cadaveric studies in which investigators had to release several additional ligaments, including the spring ligament, talocalcaneal ligament, plantar fascia, and long and short ligaments, to recreate the structural collapse associated with advanced PTTD.1,2 In other words, if there is already a visible abduction of the forefoot and PT tendinosis, several internal ligaments-and the spring ligament in particular-have already been attenuated.
Signs and Symptoms
Obesity, hypertension, diabetes, and high-impact sports are all reported risk factors for PTTD. It is also more common in women who are middle-age to elderly. In over two-thirds of cases, PTTD occurs unilaterally, and clinical diagnosis usually reveals an obvious asymmetry between the feet, with edema and a medial bulge of the talonavicular joint on the affected side. There will also be an observable internally rotated position of the malleoli and a significant heel valgus, and palpation will reveal tenderness along the course of the tendon. In later stages, the patient will be unable to perform the single heel rise test. Radiographic examination will support the findings and help to determine the stage of the deformity and any degenerative arthritic changes to the foot structures.
There is strong evidence to suggest that equinus plays a significant role in the progression of AAF. An equinus contracture, most often associated with tight tricep surae muscles, applies excessive force on the weight bearing foot. Over time, this breaks down the midtarsal joint and the medial longitudinal arch, gradually increasing strain on the PT tendon. Physical therapy can be very helpful to stretch the gastrocsoleal complex and strengthen the PT muscle. In more severe cases, a careful tendo-Achilles lengthening (TAL) surgery may reduce some of these destructive forces.
Staging PTTD and AAF
Several classification systems have been developed and refined to stage the dysfunctions. Each system follows the progression of foot collapse based on multiple factors, including the condition of the posterior tibial tendon, the position of the hindfoot, and the flexibility of the deformity.
Stage I: In the mildest cases, noticeable structural changes in the foot may or may not be visible. There will be a flatfoot condition, but if the deformity has not progressed too far, the patient may be able to complete the heel rise test. The primary symptom is tenosynovitis of the PT tendon. Initial treatment will include short-term immobilization with a rigid walking boot and subsequent use of a foot orthotic and supportive footwear.
Stage II: Visible changes occur in the foot structure due to tendon attenuation and the loss of function of one or more of the critical ligaments in the hindfoot. The patient will have difficulty performing, or be unable to perform, the single heel rise. Inversion strength of the hindfoot is compromised. Foot orthotics may help, but with the loss of hindfoot ligament integrity, it may be necessary to consider fitting the patient with some type of AFO that provides control above and below the ankle joint. Physical therapy can also help to improve strength and restore some loss of range of motion.
Stage III: The deformity becomes rigid and the patient cannot perform the single heel rise test. Radiographs reveal arthritic changes starting to occur. Ankle and rearfoot motion needs to be severely restricted; gauntlet-type braces may be necessary. Surgical options such as an osteotomy, a fusion, or arthrodesis need to be considered.
Stage IV: This is an end-stage deformity; there is complete tear or rupture. Surgery, if feasible, and/or conservative bracing are necessary.
It is important to remember that all treatment options need to be considered across each stage. There are multiple factors to consider, including the patient’s weight, activity level, general health, and commitment to rehabilitation. A patient with a dysfunction classified as stage III or IV and who has a low activity level may respond surprisingly well to conservative measures, whereas bracing may not be successful for a highly active patient with a stage II diagnosis.
Johnson and Strom’s initial work laid out the major stages as I-IV.3 Bluman et al. subsequently developed subcategories for stage II.4 More recently, Raikin et al. created a novel and comprehensive system that separately grades the effects of AAF on the rearfoot, ankle, and midfoot across each stage, referred to as the RAM Classification.5
Treatment for PTTD
At the outset, patients will usually have pain, tenderness, and swelling along the PT tendon. Ice therapy for 20 minutes three times per day should help to reduce inflammation. Physicians may also prescribe nonsteroidal anti-inflammatory medications.
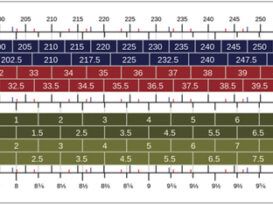
In mild cases, custom foot orthotics should be considered. Orthotics with a high medial flange will help support the entire midfoot. The orthotics can be made from thermoplastics, although not all patients will be able to tolerate the rigid control. Accommodative orthotics can be made from Thermocork or EVA, again incorporating a high medial flange to prevent midfoot collapse. Posting extrinsically provides medial varus support. Incorporating a slight heel raise often helps as it will decrease tension in the Achilles tendon if equinus is present. Requesting a Kirby heel skive in the cast will also shift ground reaction forces to the medial plantar foot.
The midfoot collapse associated with AAF and subsequent medial deviation of the STJ axis requires that the patient wear shoes with firm shanks and stiff counters. Hiking boots are ideal: The strong counters, an upper that extends well above the malleoli, lace closures, and firm soles provide better control for the entire foot. In addition, boots with removable inlays have the space necessary for custom orthotics. There are shoe modifications, such as a Thomas heel (an extension of the medial heel), a medial flare, or an external medial buttress that may help stabilize the foot.
More advanced cases or more active patients will need additional support. One of the first principles in orthotics is to control painful or pathologic motion while allowing beneficial motion. Short articulating AFOs such as the Richie Brace® have the advantage of applying some correction across the talocrural joint while still allowing transverse-plane rotation of the lower leg. Patients who are heavier or those at a more advanced stage of dysfunction may need a sturdier plastic-in-leather or Arizona®-type ankle gauntlet. Traditional thermoplastic AFOs that exert force above and below the ankle can limit motion in all three planes. In later stages, as forefoot abduction becomes prominent, it may help to extend the lateral wall of the AFO and hold the foot straight.
The literature indicates that especially in the early stages, PTTD can be managed quite successfully using combinations of foot orthotics, proper footwear, AFOs, and physical therapy. Depending on the severity of the case, results may be seen in as little as six weeks or may take up to a year. Surgical treatment can be reserved for those patients who fail an adequate trial of conservative measures.
References
- Deland, J. T., S. P. Arnoczky, and F. M. Thompson. 1992. Adult acquired flatfoot deformity at the talonavicular joint: Reconstruction of the spring ligament in an in vitro model. Foot & Ankle International 13 (6):327-32.
- Deland, J. T., R. J. de Asla, I. H. Sung, L. A. Ernberg, and H. G. Potter. 2005. Posterior tibial tendon insufficiency: Which ligaments are involved? Foot & Ankle International 26 (6):427-35.
- Johnson, K. A., and D. E. Strom. 1989. Tibialis posterior tendon dysfunction. Clinical Orthopaedics and Related Research 239:196-206.
- Bluman, E. M., C. I. Title, and M. S. Myerson. 2007. Posterior tibial tendon rupture: A refined classification system. Foot and Ankle Clinics of North America 12 (2):233-49, v.
- Raikin, S. M., B. S. Winters, and J. N. Daniel. 2012. The RAM classification: A novel, systematic approach to the adult-acquired flatfoot. Foot and Ankle Clinics of North America 17 (2):169-81.