Many O&P practitioners are directly involved in multi-specialty teams at wound care centers and diabetic clinics. Healing chronic wounds takes time, patience, skill, and a good deal of cooperation. The patients often present with complicating medical histories such as co-existing medical conditions, or prescription drugs that interfere with healing. They may also have a poor quality of life and display symptoms of depression. Against this backdrop, the team must decide the best approach to dressing, off-loading, and closing open wounds.
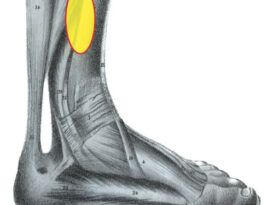
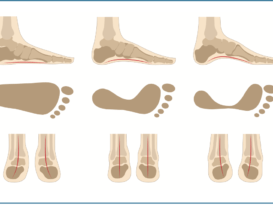
Although many factors, such as advanced diabetes, neuropathy, peripheral arterial disease (PAD), and poor biomechanics, play a role in the development of plantar foot ulcers, pressure is considered a major cause in the eventual breakdown of the skin. Pressure is defined as the application of a force over a given area [Pressure = Force/Area]. The presence of a bony prominence or the effect of wearing tight-fitting shoes can elevate pressure locally. Shear also plays a part in skin breakdown. Shear can be defined as an external force acting parallel to a plane. Directly related to pressure, it is the result of friction or rubbing. In terms of the foot, we can understand this as the tension and stretching of the skin that occurs when there is movement against a surface. The early signs of skin trauma due to shear include redness, abrasions, and blisters. The friable skin of individuals with diabetes is especially vulnerable to shear.
Once an ulcer has developed, the goal is to close the wound by eliminating or sufficiently reducing the pressure and shear. This is achieved by increasing the total contact area, in effect spreading out the load or reducing the force. Given the statistics of poor patient compliance, the practitioner needs to choose the most appropriate device carefully. In a Podiatry Management article (August 2010), James McGuire, PT, DPM, CPed, CWS, FAPWCA, associate professor in the Department of Podiatric Medicine, Temple University School of Podiatric Medicine, Philadelphia, Pennsylvania, cites a “transitional approach.” He favors using several different off-loading devices, moving the patient through a course of treatment. The following discussion summarizes some of the more widely used off-loading devices.

Charcot Restraint Orthotic Walker (CROW). Made with rigid polypropylene, it has a fully lined, removable, multi-density insert and external rocker sole.
Bed Rest: For the worst cases, a physician may recommend bed rest to fully off-load an affected limb. However, most patients will not fully adhere to this prescription, and they will continue to ambulate. The combination of impracticality and potential unhealthy side effects often overshadows any benefits.
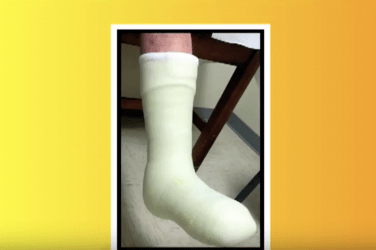
Total Contact Cast (TCC): The TCC has long been considered the best method for off-loading and healing open wounds. The TCC ensures contact over a larger surface area, which decreases peak pressure at any one location. Other benefits derived from the TCC include limiting ankle motion, eliminating shear, reducing edema, and protecting the foot from trauma. The TCC also slows the gait and reduces stride length. The advantage of “forced compliance” also contributes to the success of the device.
Many studies have shown the TCC to be highly effective in treating plantar ulcers. It is not the first choice for many physicians or patients though, as it requires experience to apply and frequent removals and reapplications, which is costly in terms of time and materials. To be effective, the wound must be debrided and dressed appropriately each time a fresh cast is applied. Initially, the patient is seen within about three days to check on edema and the fit of the cast. After that he or she is scheduled every one to two weeks with the possibility that healing can occur in as little as four to five weeks. There are documented healing rates of 90 percent at 12 weeks. Contraindications for TCC include patients with PAD, active infections, fluctuating leg edema, or patients with a history of noncompliance regarding appointment protocol. TCC may not be the best choice for patients with unsteady gait.
Removable Cast Walker (RCW): Gait studies have shown that the RCW is as effective as the TCC in reducing forefoot pressure. With compliant patients, the RCW offers easy access to the wound for frequent assessment, or if application of advanced dressings is required. In addition, using off-the-shelf devices is relatively inexpensive. In cases where there is more severe deformity, a Charcot Restraint Orthotic Walker (CROW) may be prescribed to accommodate the foot and prevent the likelihood of amputation.

Instant Total Contact Cast (iTCC): The iTCC is a way to derive the wound-healing benefits of the TCC without the difficulties of multiple applications. It is constructed by wrapping an RCW with layers of fiberglass or plaster, or applying a few plastic ties to ensure continuous wearing of the device. An iTCC requires less training to administer, is easier to remove, more cost effective than a TCC, and, unlike an RCW, reveals any deviation from the treatment protocol.
Surgical Shoes: There are a variety of post-operative and half shoes that can accommodate dressings and be used in the healing process. Half shoes fully unload a portion of the foot. Although surgical shoes are inexpensive and easy to administer, studies consistently show that they are not nearly as effective as rigid cast walkers that restrict ankle motion.
Felted Foam Dressing: Podiatrists sometimes use multi-layered, felted foam to off-load plantar ulcers. The felt is applied directly to the skin with a large aperture for the wound. Patients can wear a rigid-sole, post-operative shoe and have the dressing changed weekly. The main concern with any cut-outs, either in felt or insoles, is the development of an “edge effect.” Care must be taken to ensure that the rim of the well or depression does not cause localized high pressure and further skin breakdown.
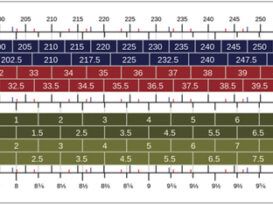
Insoles and Shoes: Both non-custom and custom orthotics and shoes are frequently used later in the cycle after stubborn ulcers have been brought under control. Total-contact, accommodative foot molds with pockets or depressions help distribute weight evenly across the entire foot. These can be incorporated into extra-depth shoes that have special features such as sole stiffeners or rocker soles to reduce peak pressures in the propulsive phase of gait. Also used to limit friction on the skin are ShearBan® and specialized, low-friction memory foams such as Plastazote® and P-Cell®.
Limited Joint Mobility and the Biomechanics of Breakdown
In normal gait, the heel contacts the ground first. As gait progresses the body passes over the plantigrade foot, the leg is in single stance, and the foot accepts full body weight as the contralateral limb goes through swing. A complex set of motions and muscle firings occurs quickly and repeatedly as we walk. One of the requirements for smooth and asymptomatic ambulation is fluid and free joint motion.
One of the side effects of diabetes and uncontrolled blood sugars is the process of glycosylation, an irreversible cross-linking of collagen and keratin. This causes a thickening of the skin, tendons, ligaments, and joint capsules. It leads to a reduction in joint flexibility and motion, otherwise termed limited joint mobility (LJM). Over time, individuals with diabetes also experience some level of muscle atrophy that deforms the toes and foot and encourages anterior migration of the plantar fat pad
If, as a result of glycosylation, the necessary ankle dorsiflexion is not available, there will be higher continuous pressure on the forefoot at the midstance and propulsive phases. Likewise, restriction of motion at the first metatarsophalangeal joint alters gait and elevates pressure beneath the hallux. These increased pressures due to LJM, in conjunction with peripheral neuropathy, are closely related with higher incidences of forefoot ulceration.
TCCs and RCWs keep the foot in the 90-degree position and work by blocking ankle joint motion. By holding the body weight back, there is a reduction in loading on the midfoot and forefoot. Shortened stride length and decreased cadence also help reduce pressure. Many of the rigid-ankle devices are made with rocker or controlled-ankle-motion (CAM) soles to smooth out the step.
Chronic open wounds need to be treated seriously due to the high cost to the patient and the community if infection occurs. To avoid amputation, the practitioner should use “maximum force” to close plantar foot ulcers and return the patient to a healthy and active lifestyle. Patients frequently resist wearing rigid casts, but their efficacy is clearly demonstrated. It is important not to compromise the choice of device by acquiescing to a patient’s lifestyle demands. Once healed, patients should be transitioned to a program of routine care and protective orthotics and shoe gear to avoid a cycle of re-ulceration.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.