This past January, The New York Times published an article in the Tuesday Science Times section titled “Close Look at Orthotics Raises a Welter of Doubts.” The article’s author briefly interviewed me for the piece. She summarized my comments as follows: “There is an abundance of evidence-hundreds of published papers-that orthotics can treat and prevent mechanically induced foot problems leading to common injuries like knee pain, shin splints, and pain along the bottom of the foot.” I was happy with the summary, but the remainder of the article generally took a skeptical look at orthotics. The writer’s specific question to me had been, “What kind of rigorous scientific evidence (like randomized, controlled clinical trials) supports the notion that orthotics, custom made or over-the-counter, can speed healing of injuries or prevent them?”
Before responding, I researched many journals and periodicals to substantiate any statements I might make. I found the whole experience quite illuminating for several reasons. First, there are plenty of papers and studies that clearly validate the use of orthotics to treat injuries and pain of the lower limb. However, not all of the studies are stand-alone positive. Some of them were conducted in conjunction with physical therapy, while others used only prefabricated orthotics, and many were inconclusive. Second, given that the evidence is not 100-percent positive, personal opinion becomes a factor in interpretation. Although we can define a problem scientifically, we often find it difficult to reconcile conflicting outcomes. This does not mean that the science is flawed but rather that the subject is more nuanced than a single cause and effect. Finally, I realized that as a profession we need to do a better job of presenting the obvious benefits and results that our orthotics and prosthetics provide. We compete with many healthcare providers and budgets for scarce reimbursement dollars. We owe it to our patients and our profession to be crystal clear about the effectiveness and direct benefits of the devices that we dispense.
Plantar Fasciitis(1-6)

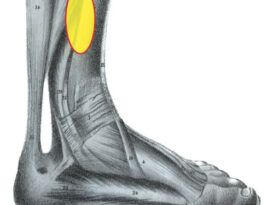
Plantar fasciitis (PF) is one of the more common foot injuries treated by foot and ankle physicians. It is a debilitating condition characterized by sub-calcaneal pain and is thought to develop due to a number of factors including abnormal foot mechanics and overuse. There are several excellent studies that show the benefits of orthotic therapy. One randomized prospective study by Lynch et al.1 evaluated 103 subjects (n=103) to compare the individual effectiveness of three types of conservative therapy: anti-inflammatory, accommodative, or mechanical. A statistically significant difference was noted between the groups: mechanical treatment with taping and orthoses proved to be more effective (70 percent reported improvement) than either anti-inflammatory (30 percent reported improvement) or accommodative (33 percent reported improvement) modalities.
Gross et al.2 investigated the impact of custom, semi-rigid foot orthotics on pain and disability for individuals with PF (n=15). They concluded that custom, semi-rigid foot orthotics may significantly reduce pain experienced during walking and may reduce more global measures of pain and disability for patients with chronic PF. Hume et al.3conducted a literature review to determine the effectiveness of foot orthoses for the treatment and prevention of lower-limb injuries. One conclusion was that customized semi-rigid foot orthoses have moderate to large beneficial effects in treating and preventing PF and posterior tibial stress fractures. They also noted that further research with randomized controlled trials is needed to establish the clinical utility of a variety of foot orthoses for the treatment and prevention of various lower-limb injuries.
References
Plantar Fasciitis
- Lynch DM, Goforth WP, Martin JE, Odom RD, Preece CK, Kotter MW. Conservative treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc. 1998;88(8):375-380. www.ncbi.nlm.nih.gov/pubmed/9735623
- Gross MT, Byers JM, Krafft JL, Lackey EJ, Melton KM. The impact of custom semirigid foot orthotics on pain and disability for individuals with plantar fasciitis. J Orthop Sports Phys Ther. 2002;32(4):149-157. www.ncbi.nlm.nih.gov/pubmed/11949663
- Hume P, Hopkins W, Rome K, Maulder P, Coyle G, Nigg B. Effectiveness of foot orthoses for treatment and prevention of lower limb injuries: a review. Sports Med. 2008;38(9):759-779. www.ncbi.nlm.nih.gov/pubmed/18712943
- Lee SY, McKeon P, Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis [published online ahead of print November 20, 2008]. Phys Ther Sport.2009;10(1):12-18. www.ncbi.nlm.nih.gov/pubmed/19218074
- Roos E, Engström M, Söderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27(8):606-611. http://www.ncbi.nlm.nih.gov/pubmed/16919213
- Scherer PR. Heel spur syndrome. Pathomechanics and nonsurgical treatment. Biomechanics Graduate Research Group for 1988. J Am Podiatr Med Assoc. 1991;81(2):68-72. www.ncbi.nlm.nih.gov/pubmed/1999801
Rheumatoid Arthritis(7-12)
Rheumatoid arthritis (RA) is a painful systemic disease that attacks all of the body’s joints resulting in inflammation and swelling, cartilage and bone breakdown, and joint dislocation. This sequence leads to skeletal loss of shape and alignment, pain, and loss of movement. The majority of patients suffering with RA will develop foot pathology, and in more than one-third of the cases, the foot will be the initial site of involvement. Typically, patients present with various combinations of metatarsalgia, rearfoot valgus, arch collapse, and first metatarsal phalangeal joint (MPJ) changes.
Hallux valgus deformity is the most commonly observed forefoot deformity in patients with RA. Budiman-Mak et al.7 conducted a five-year, double-blind, randomized clinical treatment trial comparing custom orthoses with placebos for the prevention of hallux valgus deformity in the rheumatoid arthritic foot (n=102). In a logistic regression analysis, the treatment group was 73-percent less likely to develop hallux valgus deformity compared with the control group.
Chalmers et al.8 compared the effects of custom semi-rigid and soft orthoses worn in supportive shoes, and supportive shoes worn alone, on MPJ pain (n=24). They concluded that custom semi-rigid orthoses worn in supportive shoes were an effective treatment for metatarsalgia. Supportive shoes worn alone or worn with soft orthoses did not provide pain relief for metatarsalgia.
In another randomized controlled trial of RA patients Woodburn et al.9 prescribed custom foot orthoses to 50 patients (n=98). They found that the custom-designed foot orthoses used continuously over a 30-month treatment period resulted in a reduction in foot pain by 19.1 percent, foot disability by 30.8 percent, and functional limitation by 13.5 percent.
Powell et al.10 looked at the efficacy of custom foot orthoses in children with juvenile idiopathic arthritis (JIA) (n=40). Their results showed that children with JIA wearing custom-made, semi-rigid foot orthoses with shock-absorbing posts had significantly decreased levels of pain, and increased speed of ambulation, self-rated activity, and functional ability levels compared with prefabricated, off-the-shelf shoe inserts or supportive athletic shoes worn alone.
References
Rheumatoid Arthritis
- Budiman-Mak E, Conrad KJ, Roach KE, et al. Can Foot Orthoses Prevent Hallux Valgus Deformity in Rheumatoid Arthritis? A Randomized Clinical Trial. J Clin Rheumatol. 1995;1(6):313-322. www.ncbi.nlm.nih.gov/pubmed/19078008
- Chalmers AC, Busby C, Goyert J, Porter B, Schulzer M. Metatarsalgia and rheumatoid arthritis–a randomized, single blind, sequential trial comparing 2 types of foot orthoses and supportive shoes. J Rheumatol.2000;27(7):1643-1647. www.ncbi.nlm.nih.gov/pubmed/10914845
- Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J Rheumatol. 2002;29(7):1377-1383. www.ncbi.nlm.nih.gov/pubmed/12136891
- Powell M, Seid M, Szer IS. Efficacy of custom foot orthotics in improving pain and functional status in children with juvenile idiopathic arthritis: a randomized trial. J Rheumatol. 2005;32(5):943-950. www.ncbi.nlm.nih.gov/pubmed/15868634
- Woodburn J, Helliwell PS, Barker S. Changes in 3D joint kinematics support the continuous use of orthoses in the management of painful rearfoot deformity in rheumatoid arthritis. J Rheumatol. 2003;30(11):2356-2364. www.ncbi.nlm.nih.gov/pubmed/14677177
- de P Magalhães E, Davitt M, Filho DJ, Battistella LR, Bértolo MB. The effect of foot orthoses in rheumatoid arthritis [published online ahead of print November 15, 2005]. Rheumatology (Oxford). 2006;45(4):449-453. www.ncbi.nlm.nih.gov/pubmed/16287926
Posterior Tibial Tendon Dysfunction(13-16)
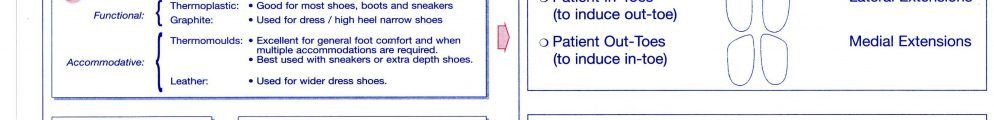
Posterior tibial tendon dysfunction (PTTD) is now considered part of a greater progressive condition called adult acquired flatfoot (AAF), which can ultimately result in significant changes in multiple foot ligaments. Contributing factors include obesity, diabetes, and age. Often, these patients are poor surgical candidates, so any and all conservative measures should be fully explored. Alvarez et al.13 conducted a study (n=47) to identify strength deficits with early-stage PTTD and to assess the efficacy of a focused non-operative treatment protocol. The rehabilitation protocol included the use of a short, articulated AFO or foot orthosis, high-repetition exercises, aggressive plantarflexion activities, and an aggressive high-repetition home exercise program that included gastrocsoleus tendon stretching. This study indicated that many patients with stage I and II PTTD can be effectively treated non-operatively with an orthosis and structured exercises.
In a long-term follow-up study (n=32), Lin et al.14 noted treatment of stage II PTTD with a double-upright AFO was shown to be a viable alternative to surgery. There was a high likelihood of adequate function, avoidance of surgery, and being brace-free at the seven- to ten-year follow-up. This represents a significant cost savings for healthcare providers and a much-improved quality of life for patients.
References
Posterior Tibial Tendon Dysfunction
- Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27(1):2-8. www.ncbi.nlm.nih.gov/pubmed/16442022
- Lin JL, Balbas J, Richardson EG. Results of non-surgical treatment of stage II posterior tibial tendon dysfunction: a 7- to 10-year followup. Foot Ankle Int.2008;29(8):781-786. www.ncbi.nlm.nih.gov/pubmed/18752775
- Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonoperative management of posterior tibial tendon dysfunction. Foot Ankle In. 1996;17(12):736-741. www.ncbi.nlm.nih.gov/pubmed/8973895
- Augustin JF, Lin SS, Berberian WS, Johnson JE. Nonoperative treatment of adult acquired flat foot with the Arizona brace. Foot Ankle Clin.2003;8(3):491-502. www.ncbi.nlm.nih.gov/pubmed/14560901
The Painful Foot(17-22)
There are many other studies that validate the use of custom foot orthoses for a variety of painful foot conditions. Burns et al.17 examined the effect of orthotic therapy for the painful cavus foot (n=154). They concluded that custom foot orthoses were more effective than a control for the treatment of cavus foot pain and its associated functional limitations.
Slattery et al.18 tested subjects (n=16) with hemophilia A and stages one through five of ankle joint damage. Over a six-week period, researchers evaluated the efficacy of functional foot orthoses. Their findings supported the use of functional foot orthoses to treat patients with hemophilia A, as significant reductions in pain levels appear to greatly improve the lives of the patients.
Likewise, studies on patients with forefoot pathologies such as metatarsalgia19,20 and functional hallux limitus21found successful conservative treatment to be viable alternatives to surgeries.
References
The Painful Foot
- Burns J, Crosbie J, Ouvrier R, Hunt A. Effective orthotic therapy for the painful cavus foot: a randomized controlled trial. J Am Podiatr Med Assoc.2006;96(3):205-211. www.ncbi.nlm.nih.gov/pubmed/16707631
- Slattery M, Tinley P. The efficacy of functional foot orthoses in the control of pain in ankle joint disintegration in hemophilia. J Am Podiatr Med Assoc.2001;91(5):240-244. www.ncbi.nlm.nih.gov/pubmed/11359888
- Postema K, Burm PE, Zande ME, Limbeek J. Primary metatarsalgia: the influence of a custom moulded insole and rockerbar on plantar pressure. Prosthet Orthot Int. 1998;22(1):35-44. www.ncbi.nlm.nih.gov/pubmed/9604274
- Kang JH, Chen MD, Chen SC, Hsi WL. Correlations between subjective treatment responses and plantar pressure parameters of metatarsal pad treatment in metatarsalgia patients: a prospective study. BMC Musculoskelet Disord. 2006;7:95. www.ncbi.nlm.nih.gov/pubmed/17147793
- Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc. 2002;92(2):102-108. www.ncbi.nlm.nih.gov/pubmed/11847262
- Hawke F, Burns J, Radford JA, du Toit V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008;(3):CD006801. www.ncbi.nlm.nih.gov/pubmed/18646168
Diabetes(23-25)
The medical costs and complications from the progression of diabetes mellitus are well understood. Protection of the neuropathic foot and offloading pre-ulcerative calluses are critical in the efforts to preventing ulcerations and eventual amputations. The use of properly designed total-contact foot orthoses in conjunction with orthopedic shoes, AFOs, cam walkers, etc. is essential. In addition to having a better quality of life, patients who continue to walk and stay active remain healthier and delay the onset of the more pernicious aspects of the disease.
References
The Diabetic Foot
- Mueller MJ, Lott DJ, Hastings MK, Commean PK, Smith KE, Pilgram TK. Efficacy and mechanism of orthotic devices to unload metatarsal heads in people with diabetes and a history of plantar ulcers. Phys Ther.2006;86(6):833-842. www.ncbi.nlm.nih.gov/pubmed/16737409
- Burns J, Wegener C, Begg L, Vicaretti M, Fletcher J. Randomized trial of custom orthoses and footwear on foot pain and plantar pressure in diabetic peripheral arterial disease. Diabet Med. 2009;26(9):893-899. www.ncbi.nlm.nih.gov/pubmed/19719710
- Bus SA, Valk GD, van Deursen RW, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev.2008;24(suppl 1:S162-180). www.ncbi.nlm.nih.gov/pubmed/18442178
These studies are only a sampling of the available literature. They clearly demonstrate the benefits of foot orthoses in treating various painful and debilitating conditions of the lower limb. In many cases, it is accepted that orthotics are not a standalone cure but, taken as part of an overall program of rehabilitation, they considerably improve function and quality of life for many patients. Certainly, more work needs to be done to refine our understanding and develop predictive models for treating specific patient groups and designing therapeutic devices. Notwithstanding, I feel that it is important that we champion the effectiveness of foot orthotics.
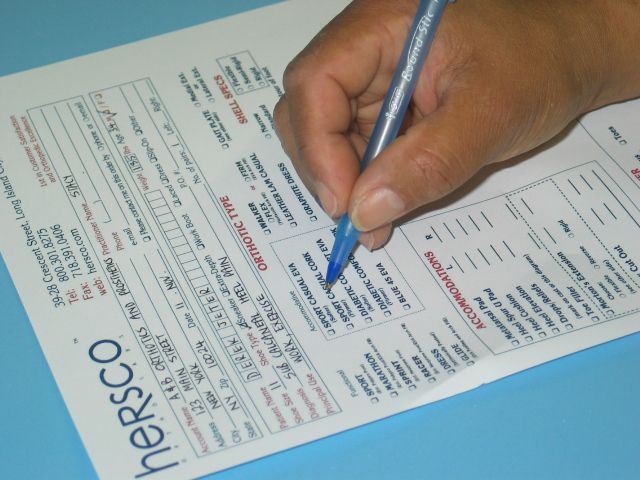
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.