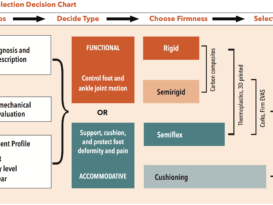
The science of fabricating and dispensing custom foot orthotics requires practitioners to make a series of clinical decisions to deliver an optimal device for each patient. In addition to following the physician’s prescription or contacting them for a discussion to develop the best solution, there are often competing objectives to be considered, such as rigidity, cushioning, and bulk. The goal is to provide the therapeutic benefits the patient needs in a device he or she will tolerate and wear. Other considerations may include longevity of the orthotic, speed of delivery, and cost. Against this background of demands there is quite an array of materials and manufacturing methods available to produce foot orthotics, which can sometimes be confusing.
 First Steps
First Steps
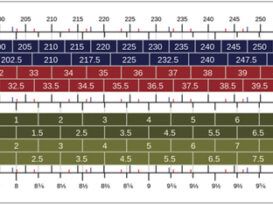
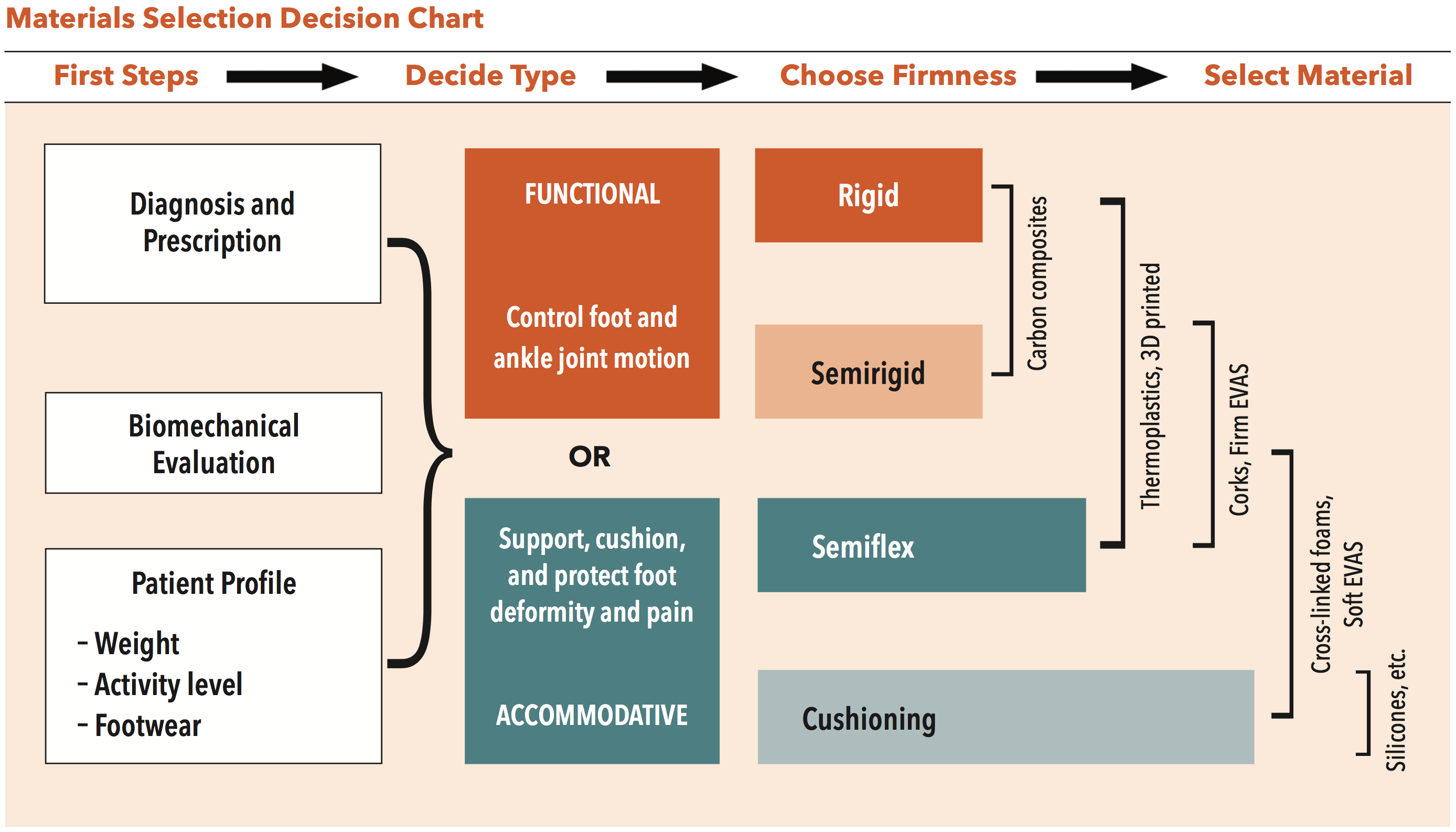
The primary consideration in the design of any foot orthotic is the physician’s prescription and diagnosis. The second factor of importance are the findings from a thorough biomechanical examination. Thirdly, criteria such as the patient’s footwear, lifestyle, and activity level also guide the design and material choices. The top section of most orthotic lab order forms requests patient information that directly influences and informs this decision-making. Among the important details are the patient’s weight, shoe size, and shoe type that allow the technician to select the best materials for the orthotic.
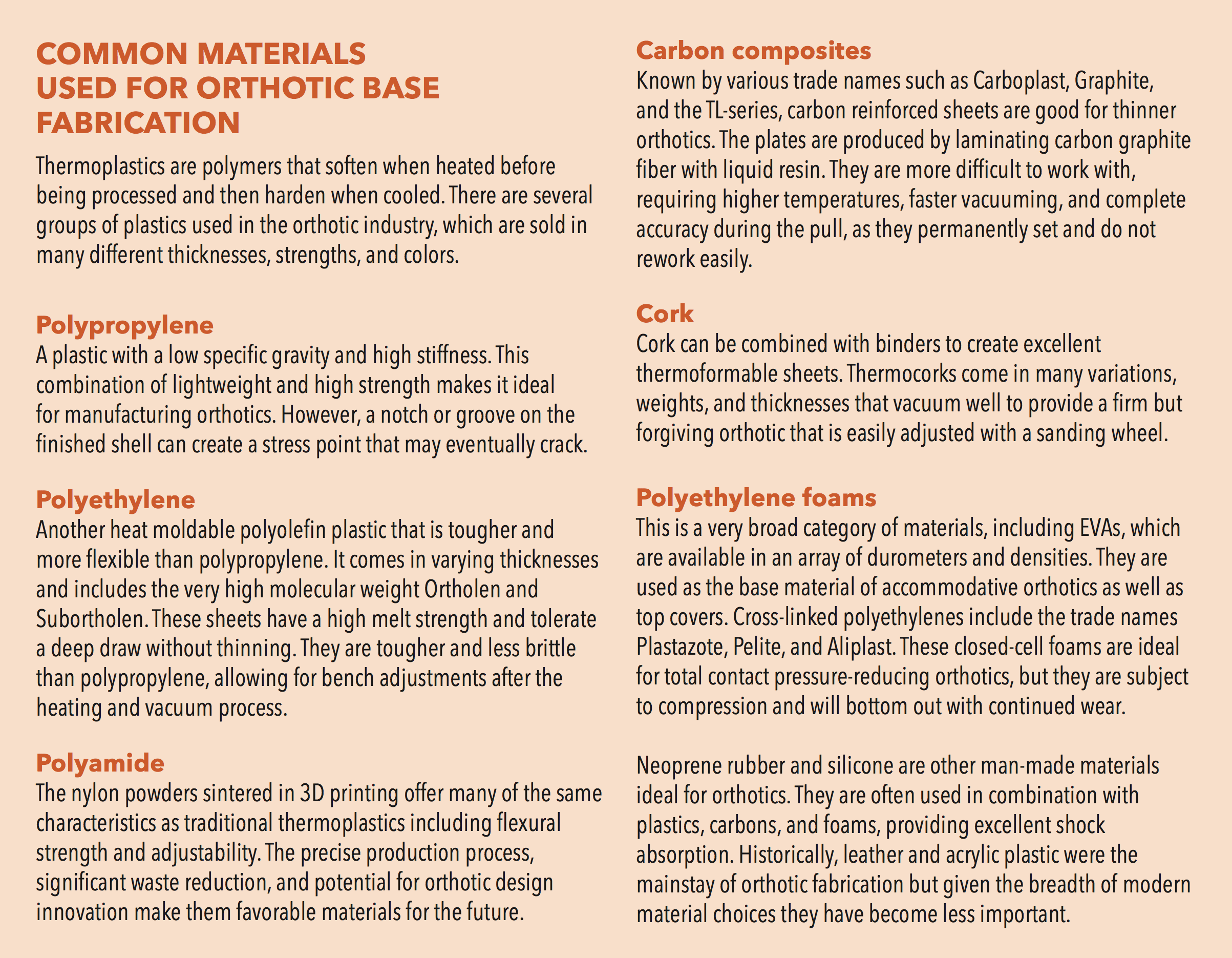
Shell specifications control the amount of support the shell provides: flexible, semirigid, or rigid. This is determined by several factors including the choice of material, the thickness of that material, the width, contour, and trimlines of the shell, and the method of manufacture.
The shoes that a patient wears strongly influence the type of orthotic that will work best. If patients experience general foot pain and wear tighter dress footwear, the orthotics need to be slimmer. Conversely, if they are very active and strictly using orthotics for athletics and training, the orthotics may only need to fit into sneakers. Ideally, well-fitting shoes with firm counters, a sensible heel height
(a heel drop of at least 10mm), and a removable inlay help ensure the success of the orthotics. Frequently, a little education is required to inform patients of the synergies of their orthotics with proper shoes. For example, the benefits of a semi-rigid functional orthotic can be diluted in a soft-soled, flat, canvas shoe.
Functional and Accommodative
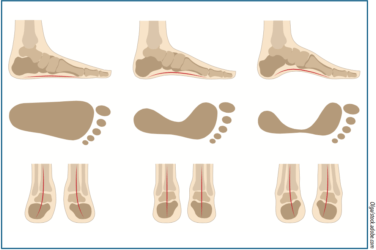
Traditionally, foot orthotics have been grouped into two broad categories. By definition, functional foot orthotics control, guide, or limit the motion of joints and muscles in the foot and ankle and proximally along the closed chain from the leg to lower back. They alter the magnitude, timing, and duration of forces acting on the foot, and as a result reduce the severity of mechanical pathology. They are proven to be very successful in minimizing pain and tissue destruction by returning the foot to a clinically normal or ideal function.
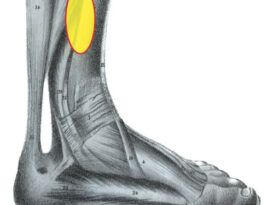
Generally, semi-rigid and rigid thermoplastic and carbon graphite orthotics have been considered functional but, based on this definition, dense foam or cork orthotics can also be functional when they achieve these objectives. Usually functional devices, regardless of the material, incorporate a deep heel cup and a good medial longitudinal arch. They are used to treat plantar fasciitis, mechanical heel pain, functional hallux limitus, pediatric flatfoot, knee pain, and a host of other pathologies that benefit from control of the subtalar joint and lower-limb biomechanics.
In contrast, accommodative devices are made from less rigid materials such as softer ethylene-vinyl acetates (EVAs), synthetic thermocorks, and polyethylene foams, which include Plastazote, Evazote, and Pelite. Although they can be bulkier, devices with these materials are usually molded to the entire plantar surface of the foot, providing noticeable comfort. Orthotics that deform under load are essentially accommodating a foot deformity rather than trying to correct it. It is also possible to make accommodative devices from flexible thermoplastics, which are sometimes reinforced with soft foams, and these hybrid devices are well tolerated by patients. Accommodative orthotics are a good choice for those with a rigid foot structure, general foot pain, or some limits in joint range of motion. They
are commonly dispensed for diagnoses such as pes cavus, rigid clubfoot, Charcot-Marie-Tooth disease, and certain cases of metatarsalgia. They are a very popular choice for older patients who do not tolerate excessive correction and are frequently used for patients with diabetes who have neuropathy and require total contact inserts.
Understanding the nature of the required device allows one to choose the most suitable material for its fabrication. There is broad overlap across categories, and the final decision may depend on other factors including practitioner preference, a patient’s previous history with orthotics, or the ability to adjust the device afterward.
The manufacturing process of thermoplastics also inherently affects the final properties of the orthotic shell. A device that is direct milled from a solid block of polypropylene will be firmer than a plate of the same thickness that has been vacuum formed. Since the milled plastic orthotic has never been oven heated, it is stiffer, and the ridge lines from the carving tool enhance its strength. For a fuller discussion
on other relevant parameters, refer to “Design Modifications for Functional Foot Orthotics,” The O&P EDGE, September 2020.
 3D Printing
3D Printing
3D printing introduces new variables into the fabrication process. Greater variations in material performance and design have become possible, opening new worlds of creativity for orthotic production. 3D printing can vary shell thickness, and therefore rigidity, under targeted regions of the foot. This allows for firm support where the load is high and a thinner flexible shell elsewhere.
Among the many types of 3D printing available, a couple are being used successfully to commercially produce foot orthotics. The simplest of these systems is fused deposition modelling (FDM). FDMs are available in affordable desktop units with a spool of polymer filament that is melted and deposited, layer by layer, onto a build platform. Beyond the physical properties of the extruded material, it is also possible to affect the characteristics of these orthotics by varying their internal latticed structure. Less dense patterns provide more cushion. The surface finish from FDM printers is a little rough and porous, so adding traditional top covers over these devices is recommended to reduce friction and prevent foreign bodies from getting caught in the open mesh.
A second additive manufacturing process widely adopted by the medical field is powder sintering. Both Multi Jet Fusion (MJF) and selective laser sintering (SLS) require a significantly higher capital investment, but they are capable of producing highly accurate parts on a much larger scale. These printers work by sintering fine plastic powders. Nylon or polypropylene is systematically fused using intense heat. The nylons are referred to by their chemical family name, polyamide (PA), and the number of carbon bonds they hold. Although PA-11 and PA-12 differ slightly in composition, they are used in the production of wheels, gears, and other demanding engineering applications that require tensile strength, ductility, and fatigue resistance. Both have been used successfully to print orthotics.
MJF and SLS technology produce smooth, strong pieces that are highly accurate and uniform. These parts are machinable and can be adjusted on sanding wheels. The process offers several important advantages. Firstly, the precision is superior to manually fabricated thermoplastics. For example, a 4mm medial heel skive will be exact, and repeatable whenever a new order is requested. This also has benefits for researchers conducting standardized studies.
Secondly, 3D printing is environmentally friendly. The additive manufacturing process only uses material required for the part with very little waste. Traditional foot orthotic fabrication creates approximately 4 lb. of waste per pair when considering the plaster positive, plastic, and casting material that gets thrown away. Even CNC milling results in approximately 2 lb. of plastic waste per pair. 3D printing with polyamides allows the powder to be recycled, reducing the waste to 5-6 oz. per pair. Additionally, PA-11 is not a petroleum-derived plastic. It is formulated from the oil of castor beans, which is a biorenewable resource.
Finally, there will likely be a lot of innovation in orthotic design as physicians and researchers investigate new possibilities to vary shell properties. No longer constrained by uniform material thickness, orthotic shells can be made simultaneously flexible and strong, potentially targeting specific phases of gait. Likewise, using multi-density honeycomb support structures FDM shells could be calibrated to deform in a non-linear manner.
This is a broad sketch of choices for the shell or base material of foot orthotics. There are many more options when it comes to padding, cushions, and top covers, including foams, gels, and multi-laminates.1 A knowledge of the spectrum of material choices allows clinicians to design and develop the ideal orthotic for each patient’s needs.
 Séamus Kennedy, BEng (Mech), CPed, FAAOP(A), is president and co-owner of Hersco Ortho Labs, New York. He can be contacted at seamus@hersco.com or by visiting www.hersco.com.
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A), is president and co-owner of Hersco Ortho Labs, New York. He can be contacted at seamus@hersco.com or by visiting www.hersco.com.
References
- Caselli, M. A. 2004. Orthoses, Materials, and Foot. Podiatry Management.