Understanding Hallux Valgus
Hallux Valgus (HV) is a progressive deformity of the foot, recognized by the medial projection of the 1st metatarsal and the abduction of the hallux away from the longitudinal axis of the foot. Patients’ initial concerns are usually cosmetic. They may also face difficulty when buying regular shoes, and frequently report irritation and blistering from shoe wear. As the condition progresses shoe fit becomes a major problem as most shoes will be too tight across the ball of the foot – but switching to a wider shoe to accommodate the bunion often leaves the new shoe loose at the heel. Increased pain when ambulating may result in less activity leading to a decrease in overall health. Due to different measuring criteria it is difficult to accurately determine the prevalence in the general population. In one meta-analysis conducted in 2010 it was estimated at 23% in adults 18-65 years old, and 35.7% in elderly people (>65 years)1. It is seen to affect women at a rate at least twice as high as men, and several studies also confirm the presence of HV in children.
In the last decade the thinking about HV has evolved significantly to consider it a triplanar deformity, i.e. a pronation of the first metatarsal bone and a valgus deformity of the phalanx.
Several studies have been conducted that examine the rotated position of the head of the first metatarsal. This article looks at the pathomechanics (changes in normal biomechanical function as a result of trauma or disease) that contribute to the condition.
History and Etiological Factors
Over the past 100 years, many causes have been suggested for the slow abducting migration of the big toe. These include excessive joint mobility, inherited factors, the presence of flatfoot, and poorly fitting shoes. Despite plenty of research, at present there is no single pathway or contributing factor that predicts the development of Hallux Valgus. However, multiple risk factors associated with HV have been isolated and classified as either
extrinsic or intrinsic (Table 1).

Inappropriate, and especially narrow, footwear is implicated in the development of HV. It is often cited that there is a far lower prevalence of HV in unshod populations—the incidence is up to 15 times higher in shoe-wearing societies. But not all women who wear high heels or shoes with a narrow toe box develop bunions. Similarly, although people wear identical shoes (left matches right) they will often present with a unilateral bunion. Accordingly, shoes are considered a factor in the progression rather than as the cause of the condition. The emergence of HV is typically a slow process and it is thought that high levels of repetitive activity also contribute to the deformity.
The intrinsic factors include sex, ligamentous laxity, genetics, and age, although none of these is definitive. Researchers have investigated ligamentous laxity and, while not conclusive, there are indications of a higher incidence of generalized hypermobility in subjects with HV. However, the presence of hypermobility does not necessarily make it the primary predisposing factor. Several works cite an involvement of positive family history in at least two-thirds of cases, although the question remains whether patients inherit the bunion or just the foot function leading to the condition.
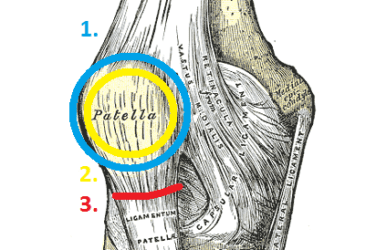
More recently, metatarsal morphology (examining the form and structure), including the angle of the first metatarsal and the dimension, shape, and orientation of the head, have been studied closely to determine if foot anatomy can provide further clues. One paper looked at the length of the first metatarsal relative to the second and found that 77 percent of 110 patients with HV had a first metatarsal that was equal to or greater in length than the second.3 A longer first metatarsal would typically result in greater dorsiflexion forces, creating what the authors referred to as a “buckle point.” The static stabilizers around the first metatarsal phalangeal joint (MPJ) are also abnormal in HV patients. Again, it is believed this is not itself the causal factor but rather a consequence.


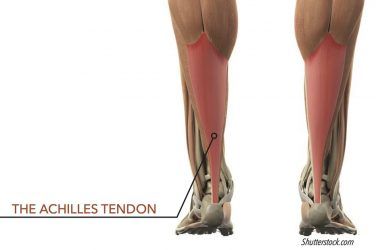
A tight Achilles tendon also plays a role, as it is can be a primary cause of pronation that influences foot function. The presence of equinus sets up a sequence of events that can block first MPJ motion, and it has been proposed that HV is one potential compensation for this blockage.4 In general, equinus is defined as any restriction in ankle joint motion that limits ankle dorsiflexion to less than 10 degrees. (Author’s note: For a more complete discussion of equinus, see “Equinus,” The O&P EDGE, April 2013.)
Development of the Deformity
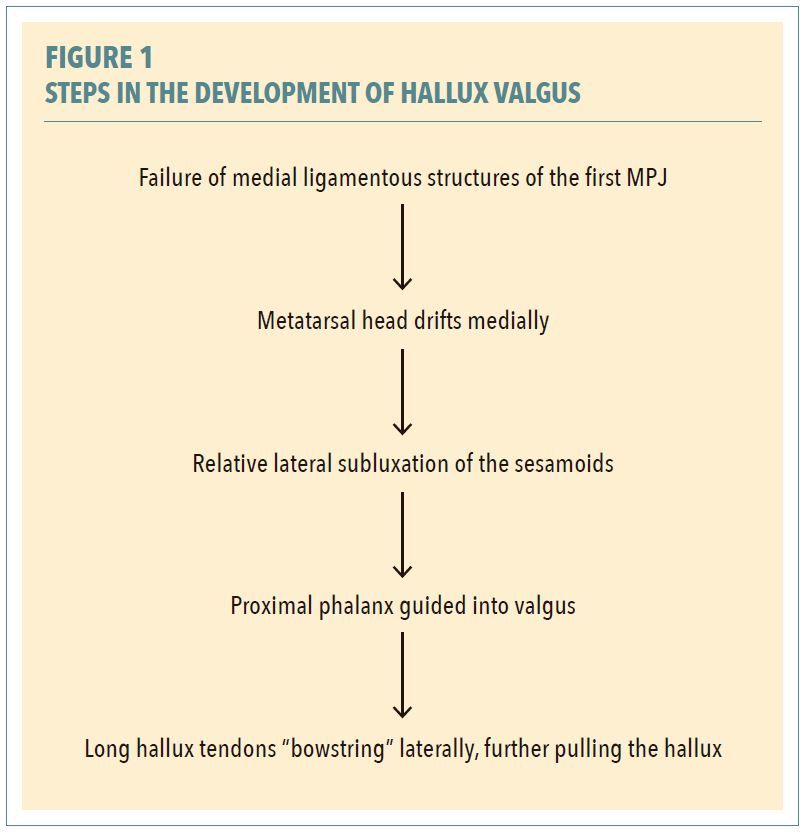
Given the presence of one or more of these predisposing factors, it is believed that Hallux Valgus occurs in steps. The exact sequence is not well understood and some of these steps may occur in parallel.2,5 Failure of the medial supporting structures of the first MPJ is considered the primary event. The metatarsal head can then drift medially but, beneath it, the more stable sesamoids remain in place. As the hallux, at its base, is tethered to the sesamoids, this encourages the phalanx into valgus. Due to the pressure of footwear, a bursa can develop on the medial side of the first metatarsal. Since the big toe is now at an angle, the long hallux tendons are no longer pulling straight along the shaft of the metatarsal; they are more like the strings of a bow. This off-center pull, enhanced by tapered or pointy shoes, is analogous to guiding the reins on a horse sideways to move in a desired direction. The gradual imbalance in tendon tension exacerbates the deformity, facilitating the process of slowly pulling the hallux further into valgus. These component steps of development are summarized in Figure 1.
A biomechanical model outlining a pathway for the development of HV was proposed in the 1990s.4 Essentially, it investigates the role of functional hallux limitus (FnHL). FnHL is the inability of the first MPJ to dorsiflex sufficiently during gait, even though normal joint motion is available when non-weight bearing. In normal gait, when heel lift occurs there should be an equal amount of dorsiflexion at the big toe. The theory can be summarized as follows: Patients with certain foot types (everted calcaneus, forefoot valgus, plantarflexed first ray) have higher ground reaction force under the first metatarsal head. If this leads to FnHL, joint motion is severely restricted. Some feet will overcome this blockage by finding a compensation at the midtarsal joint. But others are unable to find adequate compensation, and the first ray is forced further into dorsiflexion. Based on several other factors it will result in either HV or a hallux rigidus. The concept fits well with some of the previously cited intrinsic risk factors that include pes planus, FnHL, and equinus. (Author’s note: For a more complete discussion of the theory, refer to Chapter 4 in Recent Advances in Orthotic Therapy, by Paul Scherer, DPM.)
Orthotic Solutions
The Hallux Valgus deformity is one of the most common problems podiatrists face, with patients reporting swelling, inflammation, and foot pain. It has been linked to functional disability, impaired gait, poor balance, and falls in the elderly. Although it is not possible to reverse the deformity, its progress can be retarded in the early stage. Custom foot orthotics, if indicated, should be fabricated from a neutral slipper cast with the first ray plantarflexed. Requesting a rearfoot posted orthotic with a medial heel skive and a reverse Morton’s extension will provide the best opportunity to maintain motion of the first MPJ.
DESPITE PLENTY OF RESEARCH, AT PRESENT THERE IS NO SINGLE PATHWAY OR CONTRIBUTING FACTOR THAT PREDICTS THE DEVELOPMENT OF HV.
In later stages, it becomes difficult to get a proper shoe fit and the condition cannot be reversed unless the patient undergoes surgery. It is estimated that over 200,000 bunion correction surgeries are performed in the United States annually. In addition to the severity of the deformity, any decision to operate should consider the patient’s quality of life. As a palliative, orthotics sometimes help improve quality of life, providing short-term symptomatic relief and possibly extending the time before surgery.6 Eventually the hallux may even drive the second toe up and those patients usually require extremely wide shoes with very high toe boxes. Shoes with stretchable neoprene uppers may accommodate these foot types. Finally, the patient may have to opt for custom shoes to get an adequate fit. Custom-molded shoes can be made to any foot shape and can incorporate features such as rocker soles to aid ambulation.
Conclusion
It is vital to understand the contribution and relationship of the many risk factors associated with HV if we are to attempt to control and prevent this costly and debilitating deformity. This is important as it is documented that in 40 percent of juvenile patients the deformity develops before age ten, and approximately 50 percent of all adults with HV note that their deformity began in adolescence.
Given the high long-term medical costs of treating HV, it would seem sensible to validate the pathway of its development and build a protocol for early intervention. If supported, physicians and other practitioners could screen for the deformity in children. This would require examining for the causative factors and then prescribing appropriate measures such as proper footwear and functional orthoses.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via email at seamus@hersco.com or by visiting www.hersco.com.
References
-
- Nix, S.E., M. L. Smith, and B. T. Vicenzino. 2010. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. Journal of Foot and Ankle Research 3:21.
- Perera, A. M., L. Mason, and M. M. Stephens. The pathogenesis of hallux valgus. The Journal of Bone and Joint Surgery. American Volume 93(17):1650-61.
- Mancuso, J. E., S. P. Abramow, M. J. Landsman, M. Waldman, and M. Carioscia. 2003. The zero-plus first metatarsal and its relationship to bunion deformity. The Journal of Foot and Ankle Surgery 42(6):319-26.
- Roukis, T. S., P. R. Scherer, and C. F. Anderson. 1996. Position of the first ray and motion of the first metatarsophalangeal joint. Journal of the American Podiatric Medical Association 86(11):538-46.
- DeHeer, P. 2018. Pertinent principles in treating juvenile hallux valgus. Podiatry Today 31(2):48-53.
- Torkki, M., A. Malmivaara, S. Seitsalo, V. Hoikka, P. Laippala, and P. Paavolainen. 2001. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA 285(19):2474-80