Chronic low back pain (LBP) is one of the most common reasons people will see a doctor or miss days at work. According to the World Health Organization, the lifetime prevalence of LBP in industrialized countries is estimated to be 60-70 percent. As it is often difficult to pinpoint a specific cause, its development is frequently considered to be multi-factorial. What is clear is the immense economic burden of the condition, which by some estimates exceeds $100 billion annually.
Etiology
The National Institutes of Health’s Low Back Pain Fact Sheet lists five groups of causes that contribute to chronic LBP1 . These include congenital issues, injuries and trauma, degenerative problems, nerve and spinal cord problems, and effects related to other diseases. Although this list is extensive, a significant percentage of cases cannot be ascribed to a particular cause or incident but are generally associated with repetitive stress and postural statics and dynamics. Aberrations in static alignment and gait dynamics play an underappreciated role affecting skeletal posture and our muscles’ ability to hold the body upright both in stance and gait.
Posture
Good posture is difficult to define scientifically, but it consists of several factors, and it can be known by its effects. Posture should be effortless, painless, and non-fatiguing, and a person should be able to maintain it for the duration of regular daily activities2. It should also require the least amount of energy. The two most important relationships in the determination of good posture are the intersection of the line of gravity with the spinal column and the lumbosacral angle. Subjectively, it may include an aesthetic component of “acceptable appearance,” but this goes beyond the concern with function.
Factors affecting posture include hereditary characteristics such as muscle tone, ligament laxity, and familial traits; structural abnormalities, whether congenital or acquired; and habit, training, and lifestyle. It is important to consider this third group as our modern, computer-dominated workplace leaves many of us sitting most of the day—shortening the iliopsoai, hamstrings, and gastroc-soleus muscle groups. Habitual use of handheld devices also leads to drooping heads and a slouching posture. Beyond these considerations, evolution remains the underlying factor in human posture. The transition from quadruped to upright bipedal gait centered the support of the body and its mobility at the pelvis. It is the junction that acts as the mobile link between the legs and the base of support for the upper body—a crossroads of opposing muscles and forces.
Conceptually, the body is supported by an inert column of bones with several muscles innervating to maintain static alignment. In the lower leg, one of the functions of the gastroc-soleus is to keep us from tilting and falling forward. The iliopsoai are important hip flexors and low back stabilizers that originate in the lumbar spine and iliac fossa and insert into the lesser trochanter of the femur. In stance, the iliopsoai prevent hyperextension of the hip but can also increase lordosis, curvature in the lumbar spine, creating anterior tilt of the pelvis. In the absence of good posture, these muscles fire more frequently, which is potentially fatiguing. The iliopsoai are also crucial to gait, particularly in pre-swing, and if they tire or spasm, they affect the lumbosacral angle. An increased lumbosacral angle leads to posterior facet impingement and spinal compression.
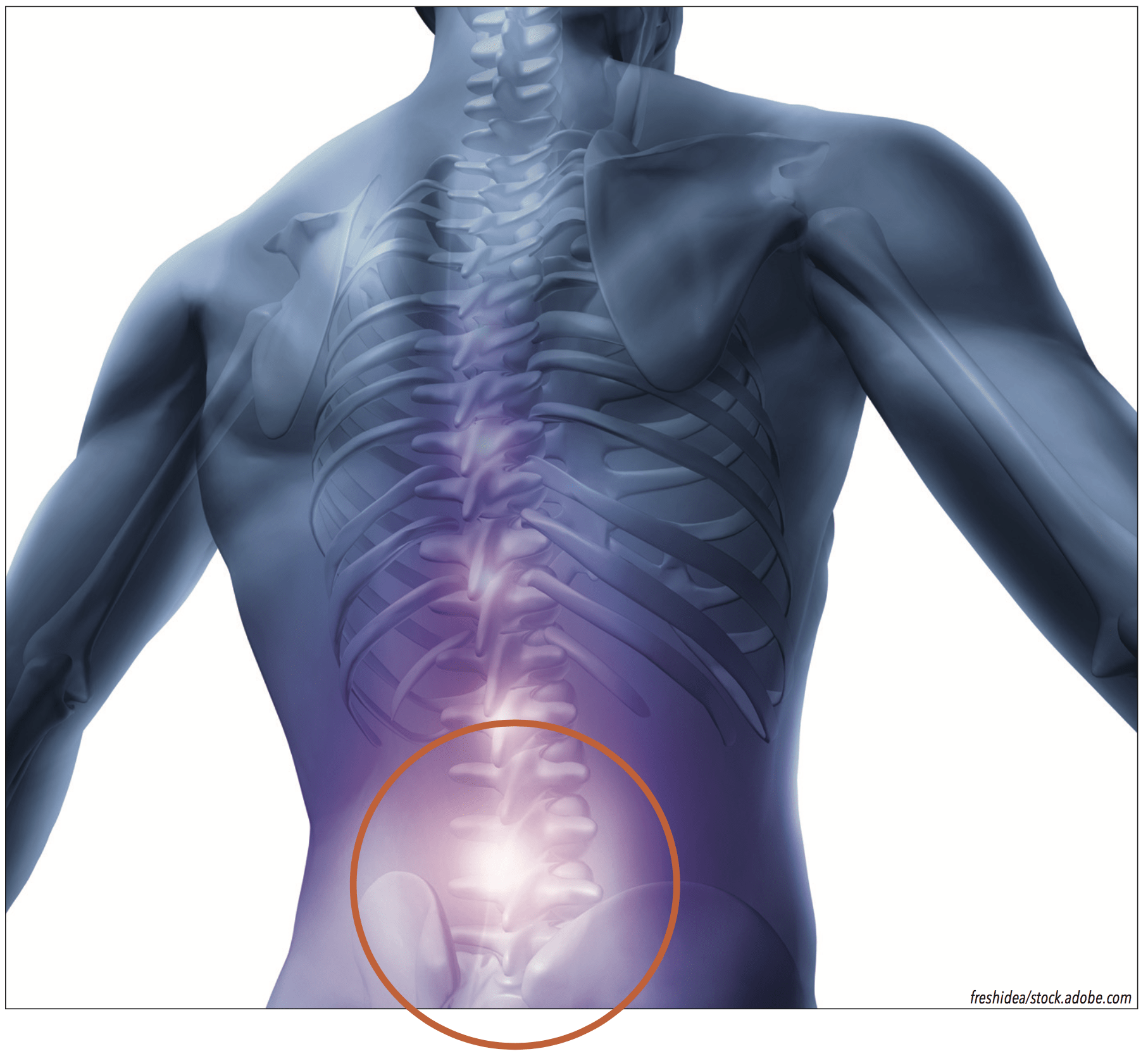
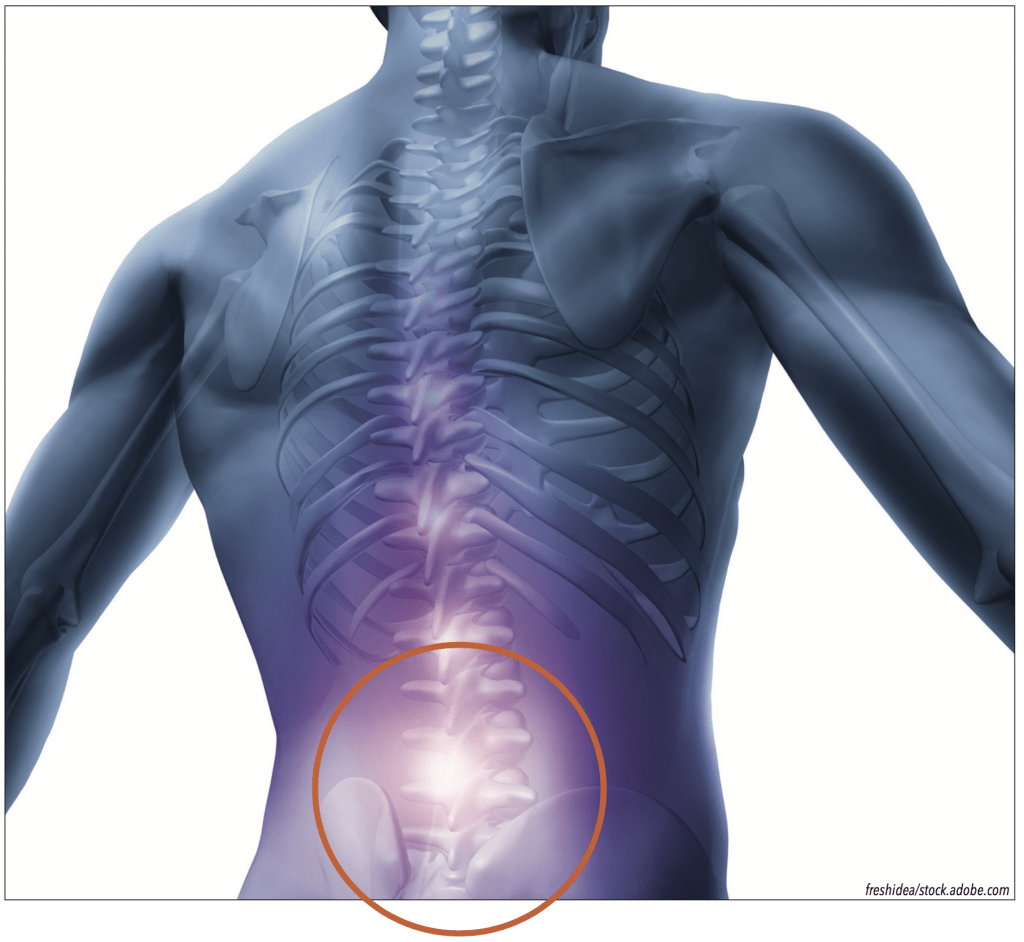
Pronation
It is not surprising that foot pronation has been linked to LBP. In one study, healthy subjects stood on everting lateral wedges of various angles and then internal leg and hip rotations were measured as well as anterior pelvic tilt3. The results indicated alignment of the lower limb up to the pelvic girdle can be altered by forces acting on the foot. Foot eversion secondary to pronation leads to internal tibial rotation and knee flexion. This in turn causes hip flexion and anterior pelvic tilt causing lumbar lordosis to compress the lumbar vertebrae (Figure 1). The chain of events is easily demonstrated when patients with a flexible flat foot transition between resting calcaneal stance position and neutral calcaneal stance. When they raise the arches of their feet, they automatically outwardly rotate the lower limbs, stand taller, and reduce lumbar curvature. Underscoring the point, in a retrospective study of almost 100,000 military recruits, moderate and severe pes planus was associated with nearly double the rate of anterior knee pain and intermittent LBP4.

Symmetry
The musculoskeletal system can be modeled as a series of links or a closed chain supporting the body. Much like a tall building, when the frame is symmetrical, the load is evenly distributed. Deviations from the ideal lead to local alterations and areas of uneven pressure or force. The most obvious difference is a limb length discrepancy (LLD) where one leg is structurally shorter, or when an imbalance occurs in function. As the sacrum sits between the ilium supporting the lumbar spine, any imbalance distal to the pelvis can alter loads left to right and potentially be a source of LBP.
Observation of any asymmetry whether in stance, gait, foot type, or shoe wear pattern is a clue that some aspect of LLD or dysfunction may be present. Typically, the center of gravity shifts to the short side and patients display indications such as head tilt, shoulder or pelvic imbalance, or scoliosis. On the long side there may be noticeable knee flexion or unilateral pronation. Sometimes an almost imperceptible difference can be the genesis of issues that may arise anywhere along the limb or the lower back. (For more information, see “Leg Length Discrepancy” in The O&P EDGE, September 2019.) In a 2012 study, researchers found that in a group of 300 patients with LBP more than 70 percent presented with a LLD, and 80 percent of these had asymmetrical loading during stance5 . The researchers noted that there was a longer lasting recovery effect when these patients were also treated with a LLD correction.
Gait in the Sagittal Plane
Beyond structural alignment and symmetry, it is also necessary to consider the effects of movement and its relationship to LBP. In gait, body segments move in all three planes, but motion in the sagittal plane greatly exceeds that of the other two. In a two-part article, Dananberg describes the biomechanical relationship between gait style and lumbar stress, and he proposes that gait interruption in the sagittal plane directly contributes to LBP6,7.
Walking can be viewed as the body moving over the fixed, plantigrade foot. To assure smooth progression, the foot provides rockers as outlined by Perry and Burnfield in the classic text Gait Analysis. The heel rocker assists the initial ground contact of the foot. Motion then transfers to the ankle, which allows the body’s center of mass to move over the foot. Finally, after heel rise, the body continues its forward momentum pivoting around the forefoot and the first metatarsophalangeal joint (MPJ). Simply put: Limitation in either the ankle or forefoot rockers has a direct influence on gait.
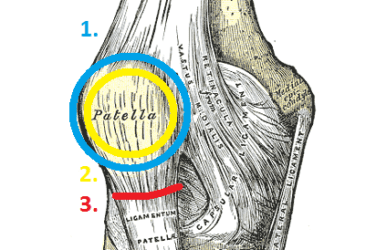
Equinus is a limitation in the motion of the ankle, defined as the inability of the foot to dorsiflex 10 degrees with the knee extended. Patients with equinus may have tight calf muscles or a bony block that impedes ankle motion and contributes to early heel rise. If you view the lower limb as a series of interconnected joints, one possible unintended consequence of early heel rise is early knee flexion, which reduces hip extension. This creates a problem for toe-off . Early in pre-swing the hip should reach approximately 15 degrees of extension (Figure 2). This is the important wind-up, analogous to a pitcher drawing his or her arm back to throw the ball. If hip extension is restricted, other mechanisms and muscles must be recruited to assist forward propulsion of the trailing limb. As the iliopsoas is a primary hip flexor, the inability of the hip to reach full extension puts repetitive stress on this muscle to assist pulling the limb.
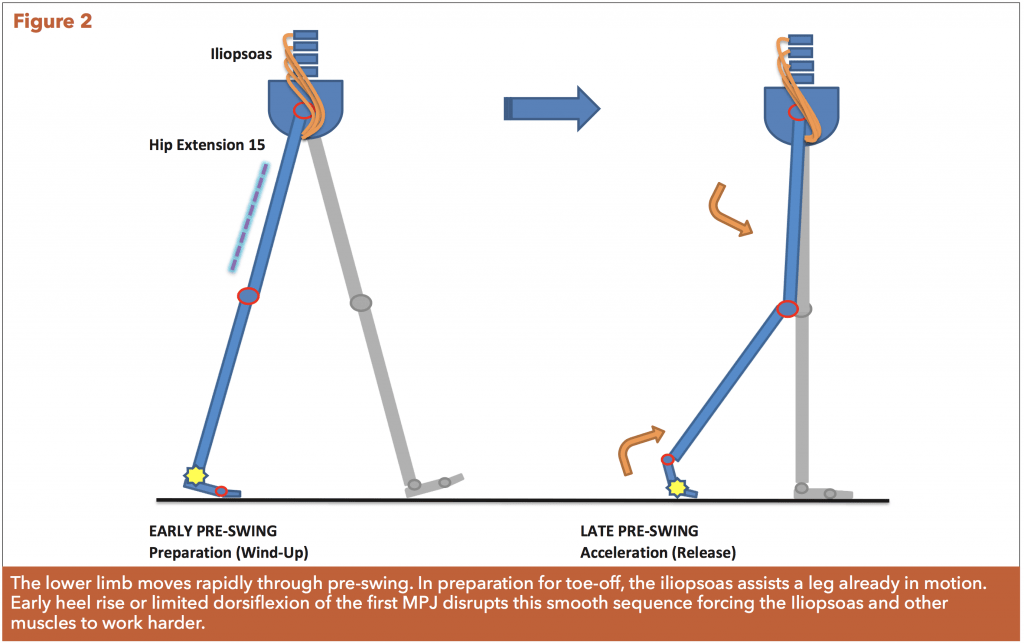
At the end of the pre-swing phase, the body’s forward motion is dependent on the function of the first MPJ. Before toe-off occurs and swing is initiated, the trailing limb should already be accelerating. Although only a portion of the forefoot is still on the ground, the ankle is rapidly plantar flexing, and both the knee and hip are flexing in preparation for swing. This is only possible if there is sufficient range of motion at the first MPJ. Hallux limitus impedes flexion of the forefoot, resulting in loss of momentum at a critical instant. It creates a sagittal plane blockage with compensations such as early toe-off or asymmetrical gait interrupting a fluid sling-shot affect. The disruption may be subtle, but in one positive outcome study of subjects with chronic LBP 100 percent of the 32 participants had either ankle equinus or functional hallux limitus8.
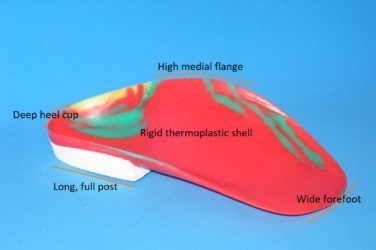
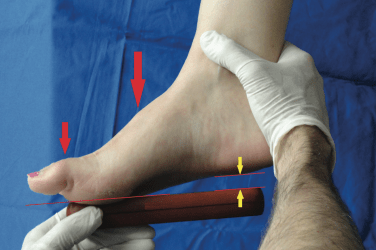
Orthotics
Orthotics can be designed to control and enhance motion and are therefore very helpful in addressing several of the issues identified as contributing to LBP. Firstly, they can counter the effects of pronation and alter posture. For patients with correctable pes planus, a semi-rigid functional orthotic with a deep heel cup will raise and maintain the longitudinal arch. This limits internal tibial rotation, realigns the leg, reduces anterior pelvic tilt, and decreases lumbar lordosis. Secondly, both structural and functional LLDs can be addressed using heel or shoe lifts, orthotics, or some combination of each. Thirdly, the harmful effects of ankle equinus can be mitigated using orthotics by encouraging a symmetrical gait pattern, optimizing the timing of key events in each step and rebalancing ground reaction forces.
Finally, mild and moderate restrictions created by functional hallux limitus can be restored with a supportive device that includes a modification such as a reverse Morton’s extension or a first ray cut-out. In cases where the first MPJ is severely arthritic and its motion is painful, it is better to dispense a rigid Morton’s extension and shoes with rocker soles. This will protect the joint while providing an external mechanical fulcrum for pre-swing. (For more information, see “Morton’s Extensions” in The O&P EDGE, May 2018.) Other treatment modalities such as physical therapy and chiropractic care seek to regain functional symmetry, muscle strength, joint motion, and proper posture and have an equally potent effect on LBP and gait. In fact, evidence suggests coupling orthotics with some form of therapy provides the best net result both for pain reduction and extending the duration of relief.
Conclusion
Many healthcare professionals believe that non-specific LBP (i.e., not associated with a trauma or obvious musculoskeletal disease) is a result of a combination of factors. If the nature of the ailment is recurring and traditional approaches have demonstrated only temporary effectiveness, there is good reason to consider the cause may be related to posture, LLD, asymmetry, or gait interruption in the sagittal plane. Although the connection is proposed rather than proven, any of these anomalies restrict ideal movement. With time they can stress or overwork the mechanisms of the lower back. Proper treatment of LBP looks beyond the symptom and seeks to restore full function, range of motion, and symmetry so the body moves naturally and pain free.
Séamus Kennedy, BEng (Mech), CPed, is president and co-owner of Hersco Ortho Labs, New York. He can be contacted via e-mail at seamus@hersco.com or by visiting www.hersco.com.
The author gratefully acknowledges the help and contribution of Joseph C. D’Amico DPM, DSc in preparing this article.
References
1. National Institute of Neurological Disorders and Stroke. National Institute of Health. 2020. Low Back Pain Fact Sheet. www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet
2. D’amico, J. C. The postural complex I. 1976. Journal of the American Podiatric Medical Association 66(8):568-74.
3. Khamis S., Z. Yizhar. 2007. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait & Posture 25(1):127-34.
4. Kosashvili, Y., T. Fridman, et al. 2008. The correlation between pes planus and anterior knee or intermittent low back pain. Foot & Ankle International 29(9):910-3.
5. D’Amico, M., P. Roncoletta, et al. 2012. LBP and lower limb discrepancy: 3D evaluation of postural rebalancing via underfoot wedge correction. Studies in Health Technology and Informatics 176:108-12.
6. Dananberg, H. J. 1993. Gait style as an etiology to chronic postural pain. Part I. Functional hallux limitus. Journal of the American Podiatric Medical Association 83(8):433-41.
7. Dananberg, H. J. 1993. Gait style as an etiology to chronic postural pain. Part II. Postural compensatory process. Journal of the American Podiatric Medical Association 83(11):615-24.
8. Dananberg, H. J, M. Guiliano. 1999. Chronic low-back pain and its response to custom-made foot orthoses. Journal of the American Podiatric Medical Association 89(3):109-17.