The word orthopaedic has two ancient Greek roots: “orthos” meaning straight or right, and “paideia” referring to the rearing of children. Thus, the original term pertained to the treatment of disorders of the bones and joints and the correction of skeletal abnormalities in children. It was probably believed, and it is generally still the case, that the earlier a deformity is addressed, the better the chances for success.
Congenital Clubfoot
This is certainly true for talipes equinovarus (TEV), more universally known as clubfoot, one of the most common congenital birth defects of the foot. Although the incidence varies somewhat according to race, TEV occurs in about one out of every 1,000 births, with the occurrence in boys being twice that of girls. Clubfoot is seen unilaterally and bilaterally; bilateral presentations make up approximately half of the cases. The etiology of the disease is not clearly understood, and many believe the causes to be multi-factorial, including genetic considerations, the intrauterine environment, and a variety of abnormalities related to the development and insertion of muscles, tendons, and ligaments. Regardless of the origin, it is important to identify congenital clubfoot as early as possible for two reasons: to begin immediate treatment to address and correct the deformity, and to rule out other, more serious diseases that may be masking as TEV, such as neuromuscular disorders, spinal tumors, or even trauma.
The typical clubfoot is turned inward and down in a classic cavo-adducto-varus presentation. Radiographic analysis will confirm the diagnosis of TEV; one will often see a talar head that is deformed and irregular, a talo-calcaneal angle that is decreased, and a talo-first-metatarsal angle that is increased. In unilateral cases, the clubfoot side is often shorter, and there are deep-seated medial skin creases. If the foot is correctable, conservative measures should begin immediately—as early as neonatally—since the deformity is progressive. Left untreated, joint contractures and accommodations will develop into a rigid clubfoot. Patients with rigid clubfoot should be referred as surgical candidates.
Flexible Flatfoot
There does not seem to be a clear consensus as to the rate of moderate-to-severe pediatric pes planus, or flatfoot, in the general population. The literature indicates a very broad range (from 3-24 percent), with several studies settling between 15-20 percent. There does appear to be a link between obese children and flatfoot, a further indication that being overweight sets the stage for more health complications later in life. The normal infant foot will not have an arch and usually displays some heel valgus. A child’s arch develops over time and should become more apparent around the age of seven.
In addressing the disorder, it is important to determine if you are dealing with a flexible flatfoot. Rigid flatfoot, caused by tarsal coalitions, usually requires surgery and will not be helped by foot orthotics. Equinus deformity can also result in the presentation of a flatfoot and should be dealt with as the primary cause before orthotic therapy begins. Finally, be aware that other motor-neuron disorders can cause flatfoot in a child and, if suspected, necessitate further investigation.
There has been an historical belief that early correction of children’s flatfoot will result in the development of an arch. This has not been scientifically tested and proven but remains a prevalent idea with some merit and considerable anecdotal evidence. Originally, pediatric pes planus was addressed using traditional Shaffer plates (high medial flange) and Whitman plates (high medial flange and lateral “clip”). These were often made from stiff sole leather, but other versions were fabricated using steel, aluminum, or Rohadur. Being flexible and correctable, a child’s foot could adapt to the rigidity and shape of these devices.
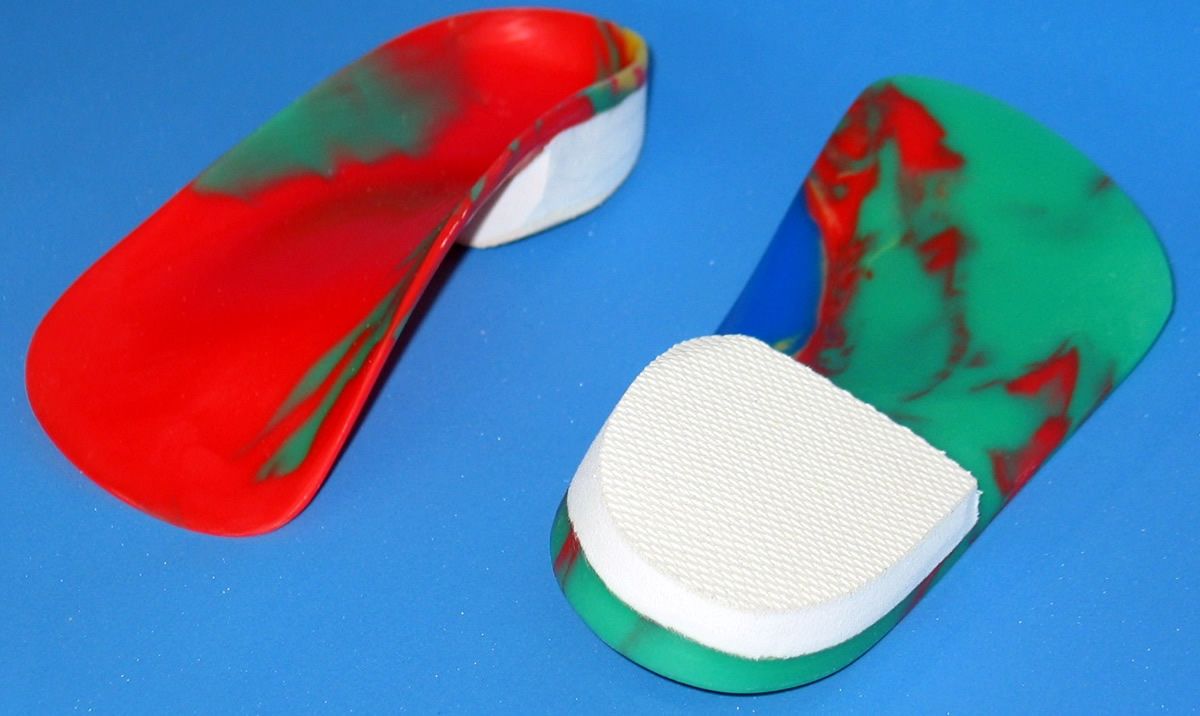
Currently, the most commonly prescribed children’s foot orthotic is the UCBL. Named for the University of California at Berkley Laboratory, where it was first developed, the UCBL is a rigid thermoplastic foot orthotic with an extra-deep heel cup (30mm+/-) and high medial and lateral walls extending distally toward the metatarsal heads. The UCBL provides classic “arch support” as it cradles the medial column and also controls the entire rearfoot. Further correction can be achieved by adding either a medial Kirby-type heel skive to the cast or a medial extrinsic post to the shell. Extra stability in pediatric orthotics is provided by extending the heel-post trim line farther distally, and having a flatter and wider shell just behind the metatarsal heads. I prefer to dispense UCBLs without any top covers because children often and easily peel them off, and because even though their toes may outgrow a full-length top cover, the shell of the device still provides adequate functional control.
 |
| Gait plates with lateral extensions, to correct in-toeing. |
Gait plates are a more specific orthotic design that are usually prescribed to correct children’s in-toeing. Originally, they were rigid flat plates inserted into the shoe to change the break point although they are now often incorporated into a regular foot orthotic. Gait plates to correct in-toe (and so induce out-toe) have a shell that ends just behind the first metatarsophalangeal joint (MPJ) on the medial side, and then extends distally past the fifth MPJ on the lateral side. This rigid lateral extension inhibits flexion of the lesser metatarsals and encourages external rotation. Gait plates work best in shoes that flex at the ball because rigid-soled shoes block their effectiveness. Gait plates to treat out-toe can also be prescribed with the extension reversed. However, many cases of pes plano valgus can be corrected using a UCBL with good medial support, which will address the compensatory pronation.
|
Séamus Kennedy, BEng (Mech), CPed, FAAOP(A) is president and co-owner of Hersco Ortho Labs, New York, New York. He can be contacted at seamus@hersco.com or by visiting hersco.com.